Reviewed by Danielle Ellis, B.Sc.Dec 18 2023
New research conducted by UCL and the Wellcome Sanger Institute underscores the pivotal role of communication between immune cells and airway lining cells in fostering healthy lung development.
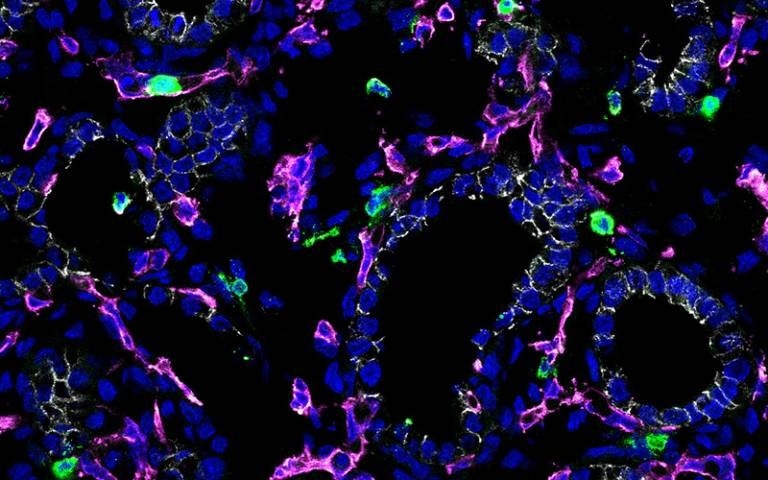
Image Credit: Marko Nikolic & Jo Barnes/University College London.
Published in Science Immunology, the study introduces a groundbreaking immune cell atlas of the developing lung, revealing earlier-than-expected coordination between the immune and respiratory systems.
This revelation prompts inquiries into the potential involvement of immune cells in the development of other organs throughout the body. Moreover, it provides fresh insights for comprehending and addressing respiratory conditions, notably chronic obstructive pulmonary disease (COPD), which globally contributes to nearly 20% of deaths in children under the age of five.
Utilizing advanced single-cell technologies, researchers from UCL, the Wellcome Sanger Institute, and EMBL's European Bioinformatics Institute meticulously mapped the progression of early fetal human lung immune cells.
Despite immune cells constituting a significant portion of both airways and mature lungs, their role in the developing organ has been relatively unexplored compared to structural or lining cell types. Recent discoveries have unveiled the presence of immune cells in human lungs as early as five weeks into development.
In their investigation spanning 5 to 22 weeks of development, the research team employed various methodologies, including single-cell sequencing and experiments with lung cell cultures.
Their objective was to ascertain whether immune cells could influence lung cell development. The findings unveiled an active role played by immune cells in guiding the growth of human lung tissue during development.
Key regulators of lung development, such as signaling molecules IL-1β and IL-13, were identified as facilitators in coordinating the maturation of lung stem cells into specialized cell types.
This groundbreaking study thus expands our understanding of the intricate interplay between immune cells and respiratory development, shedding light on potential avenues for treating respiratory conditions.
Our study shows that there is a symbiotic relationship between immune cells and the developing fetal lungs – some immune cells use the lungs as a developmental niche, preparing for exposure to an onslaught of pathogens at birth, while other immune cells help shape the lung tissue.”
Dr Jo Barnes, Study First Author, Division of Medicine, University College London
Barnes added, “Knowing that immune cells can affect tissue modeling in the developing lungs opens the door to potential regenerative therapies in not just the lung, but in other human organs.”
The scientists observed an influx of innate immune cells succeeded by adaptive immune cells. The innate cells comprised innate lymphoid cells (ILCs), natural killer (NK) cells, myeloid cells, and progenitor cells.
Regarding adaptive immune cells, the detection of both developing and mature B lineage cells, along with T cells, suggested that the lung environment is conducive to B cell development.
We now know immune-epithelial crosstalk is a feature of early lung development. This vital baseline of healthy lung development will help us understand what happens when lung developmental processes get disrupted, for example in preterm births, which can lead to respiratory deficiencies.”
Dr Marko Nikolić, Study Senior Author and Honorary Consultant, Respiratory Medicine, Division of Medicine, University College London
The discoveries fundamentally alter the comprehension of the essential immune and epithelial interactions vital for fetal lung maturation. Additionally, they imply that disruptions in early immune processes might manifest as pediatric lung diseases.
These novel insights into the mechanisms of early lung formation will further aid in the advancement of therapeutic strategies to regenerate impaired lung tissue and reinstate lung function.
The active participation of immune cells expands the possibilities for understanding and addressing impaired lung formation. What is super exciting about this mechanism is that it may well apply in other organ systems too.”
Dr Kerstin Meyer, Study Senior Author, Wellcome Sanger Institute
Source:
Journal reference:
Barnes, J. L., et al. (2023) Early human lung immune cell development and its role in epithelial cell fate. Science Immunology. doi.org/10.1126/sciimmunol.adf9988