The microbiome can identify patients with rare gynecological cancers, biliary tract cancers, and melanoma who will benefit from combination immunotherapy for various cancer types.
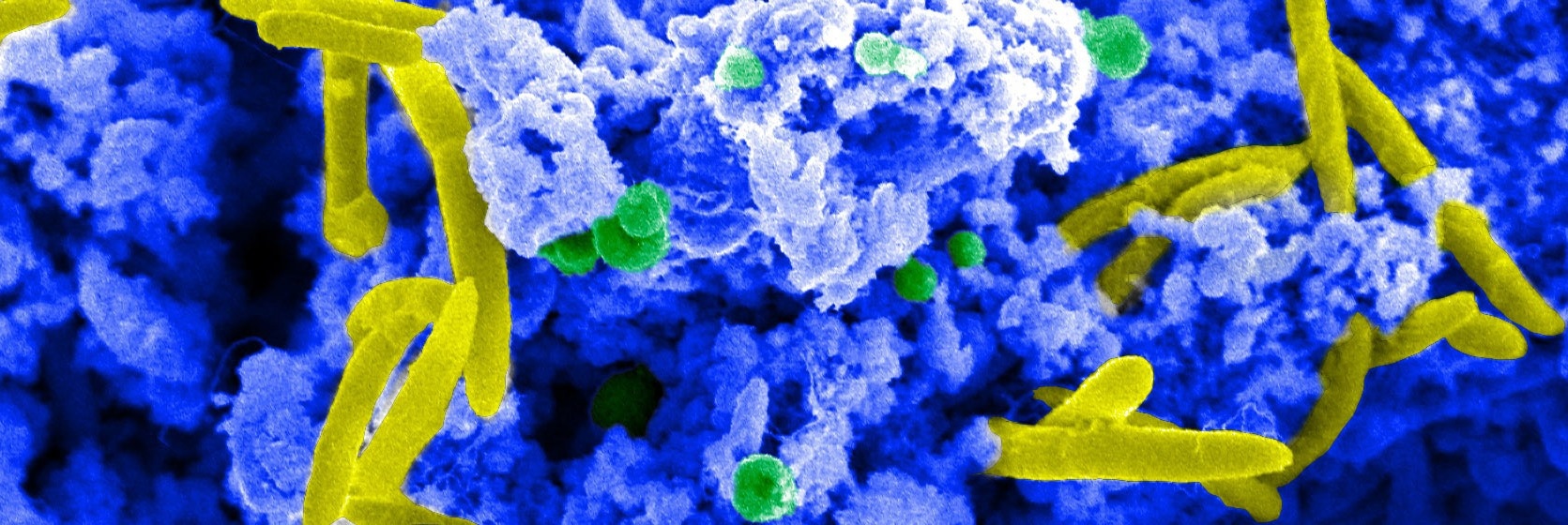
Image Credit: Dave Goulding / Wellcome Sanger Institute
Scientists from the Wellcome Sanger Institute, the Olivia Newton-John Cancer Research Institute in Australia, and associates have identified particular strains of bacteria that are associated with a favorable response to combination immunotherapy.
The study describes a signature set of microorganisms in a person’s gut flora that could help identify those who would benefit from combination immunotherapy and help explain why the effectiveness of this treatment is otherwise difficult to predict. The research was published in the journal Nature Medicine.
Future research on these bacterial strains could contribute to the creation of “live biotherapeutic products,” or next-generation probiotics, which aim to modify the microbiome to support combination immunotherapy from the inside out.
One kind of treatment called immunotherapy uses the body’s immune system to specifically target the cancer. Even though it has a high rate of success, it only benefits a small percentage of patients with a variety of malignancies. Immunotherapy can have a variety of side effects, just like any other cancer treatment.
Therefore, it helps to ensure that patients do not suffer these needless side effects for no medical benefit by being able to predict who is most likely to respond to treatment.
This study used samples from a large multi-center clinical trial conducted in Australia, where combination immunotherapy was found to be effective in 25% of patients with a variety of advanced rare cancers, such as upper gastrointestinal and biliary cancers, neuro-endocrine neoplasms, and rare gynecological cancers.
The immune checkpoint inhibitor class of combination immunotherapy was the main focus of the clinical trial. By preventing the body’s immune checkpoint proteins from functioning, these anti-cancer drugs enable the immune system to eliminate cancer cells. The immunotherapy in this instance blocked the CTLA-4 and PD-1 checkpoints.
To map every organism in the participants’ microbiomes, down to the strain level, researchers employed deep shotgun metagenomic sequencing1 using stool samples from clinical trial participants.
In those that responded well to treatment, they found several strains of bacteria, many of which had never been cultivated before. This made it possible for them to pinpoint a microbiome signature that was present in patients who showed good therapeutic response.
Furthermore, the group trained a machine learning model with this signature to predict which patients would benefit from combination immunotherapy.
After doing a meta-analysis of earlier research, they discovered that their signature can be used to predict which patients will likely benefit from combination immunotherapy for a variety of cancers, including melanoma, as well as across national boundaries.
However, the machine-learning model was unable to predict which patients would respond to treatment when it was applied to patients who received only one immunotherapy medication, which targeted the immune checkpoint receptor PD-1 exclusively.
This implies that specific therapeutic combinations may have a different relationship between gut microbiota and treatment response than others. Therefore, regardless of the type of cancer, the researchers propose that future developments in diagnostics or therapeutics based on the gut microbiome should be customized to the immunotherapy regimen.
This advancement in personalized medicine has the potential to increase the number of individuals receiving cancer treatments and match patients with the therapies that will work best for them.
Our study shows that understanding the microbiome at strain-level, not just species-level, can open up a new level of personalised medicine. Having that extra resolution is crucial if we are to understand what is happening in the human body and the interplay between cancer treatment and the microbiome. Being able to test the specific mechanisms of this relationship between specific strains and response is the next horizon in this research, and one that could benefit human health in a multitude of ways.”
Dr. Ashray Gunjur, Study First Author and Clinical Research Training Fellow, Wellcome Sanger Institute and the Olivia Newton-John Cancer Research Institute
Dr David Adams, study Co-Senior Author and Senior Group Leader added, “Rare cancers can be hard to study and treat and while immunotherapy treatment can be incredibly effective in some of these cases, it can also be unpredictable. The research shows that the microbiome impacts how well someone responds to combination immunotherapy, but that monotherapy gives a different result.”
He added, “This suggests that the microbiome should be taken into account when developing therapeutics going forward. In addition to this, there is a possibility of developing live biotherapeutic products that could provide the bacteria shown to support immunotherapy, helping the microbiome work with the patient to give them the best odds of response possible.”
Dr. Trevor Lawley, Study Co-Senior Author, Wellcome Sanger Institute said, “Our microbiomes vary from person to person, all of us containing a different ecosystem of bacteria and other organisms that shape our responses to the world around us. Our research highlights how an individual’s microbiome can predict how they will respond to cancer treatment, which can have a direct clinical impact by identifying those that would benefit the most, and aid in the design of future clinical trials.”
Oliver Klein, Study Author, Oliver Newton John Cancer Research Institute, further stated, “When considered altogether, rare cancers constitute around 20 per cent of all cancer diagnoses. Unfortunately, rare cancers are difficult to study and treat due to their infrequent nature. Combination immunotherapy can be incredibly effective in patients with rare cancers, and being able to identify factors, such as the microbiome, that are predictive of an effective response will be invaluable in making this treatment available to more patients.”
Source:
Journal reference:
Gunjur, A., et al, (2024) A gut microbial signature for combination immune checkpoint blockade across cancer types. Nature Medicine. doi.org/10.1038/s41591-024-02823-z