Reviewed by Danielle Ellis, B.Sc.Sep 19 2024
Neurological conditions can result from chronic hyponatremia, a disorder marked by low blood salt levels. In addition, osmotic demyelination syndrome (ODS), a central demyelinating illness linked to neurological morbidity and mortality, might result from the excessively quick cure of hyponatremia. Studies have connected the genesis of these problems to microglial cells.
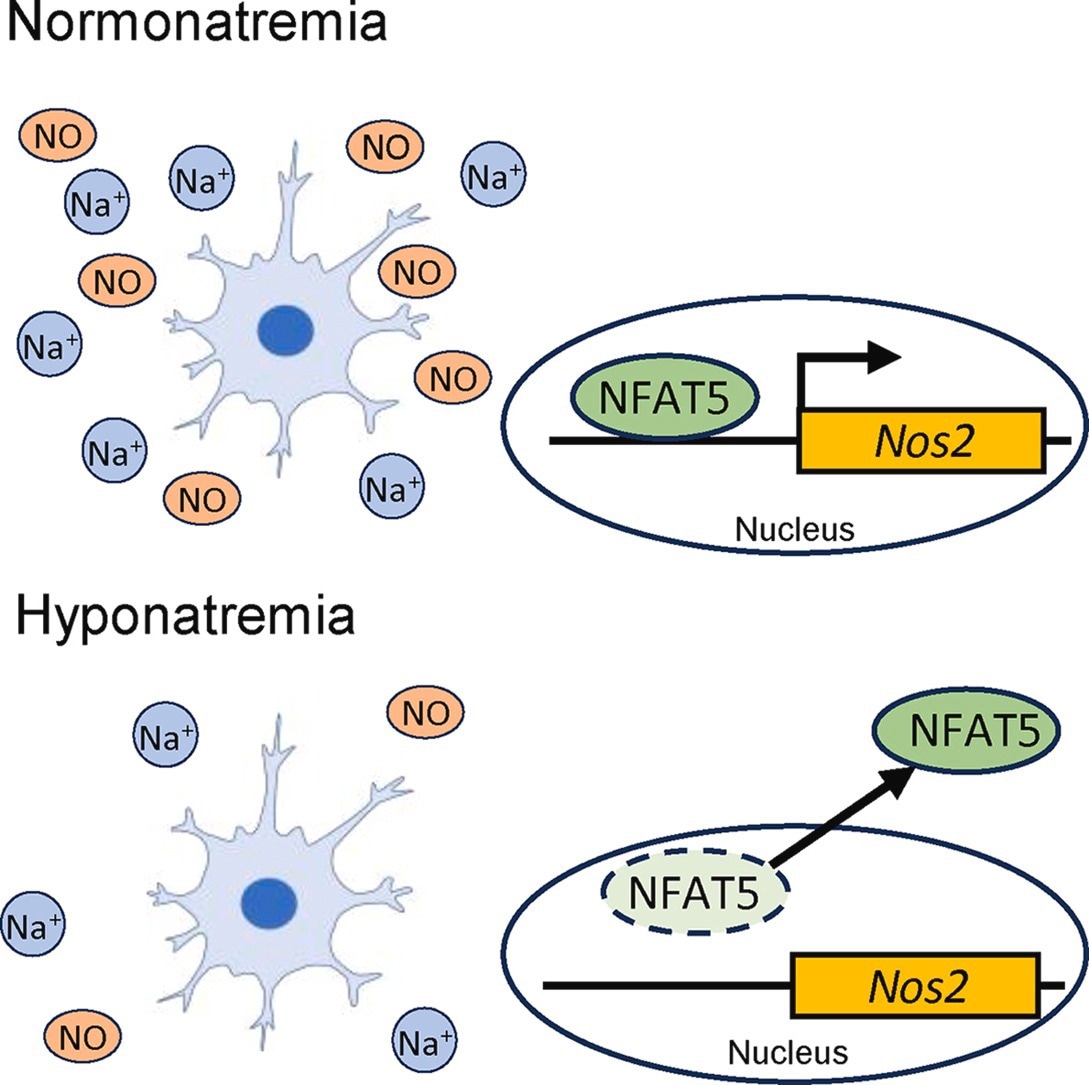 In a new study, scientists investigated the impact of low sodium concentrations and its rapid correction on nitric oxide production dependent on the expression of Nfat5 in microglial cells. Image Credit: Yoshihisa Sugimura from Fujita Health University
In a new study, scientists investigated the impact of low sodium concentrations and its rapid correction on nitric oxide production dependent on the expression of Nfat5 in microglial cells. Image Credit: Yoshihisa Sugimura from Fujita Health University
Researchers have now discovered that low extracellular sodium concentrations can inhibit nitric oxide (NO) production and the mRNA expression of nitric oxide synthase 2 in microglia.
Hyponatremia is the term for low serum sodium concentrations in blood, a common clinical electrolyte imbalance. Since the brain can effectively adjust to hyponatremia, chronic hyponatremia has historically been seen as asymptomatic in contrast to acute hyponatremia. Chronic hyponatremia can cause problems like fractures, falls, memory loss, and other mental health problems if left untreated.
However, managing the chronic illness can be challenging because it has been noted that treating hyponatremia too quickly can result in ODS. It is a neurological condition linked to neurological morbidity and death in which damage to the myelin sheath enveloping the neurons impairs nerve transmission.
Image Credit: ART-ur/Shutterstock.com
Understanding the cause of ODS is necessary to make sure that hyponatremia is treated without the side effects of the therapeutic procedure. Professor Yoshihisa Sugimura of the Department of Endocrinology, Diabetes, and Metabolism at Fujita Health University's School of Medicine discovered in a prior study that resident immune cells called microglia, which are found in the brain and spinal cord, may be crucial in the pathophysiology of ODS
Building on these discoveries, a group of scientists under the direction of Prof. Sugimura and including Haruki Fujisawa as the lead author investigated the direct effects on microglia of low extracellular salt concentrations (LS) and their quick correction.
Along with other authors, the work was co-authored by Haruki Fujisawa and Atsushi Suzuki from Fujita Health University and published in Free Radical Biology and Medicine. The researchers found that particular mRNA expression and microglia's generation of NO were both impacted by low salt levels.
Microglia migrate and monitor throughout the brain to participate in a variety of vital CNS processes, such as neurogenesis, synaptic remodeling, and myelination. When pathogens or external stimuli are present, they can get activated and release a variety of molecules, such as nitric oxide, which can start an inflammatory response.
Understanding the rather elusive effect of chronic hyponatremia and its rapid correction on microglia is crucial as it may be a potential therapeutic target for ODS and hyponatremia-related neurocognitive impairment and mental manifestations.”
Yoshihisa Sugimura, Professor, School of Medicine, Fujita Health University
The group decided to use microglial cell lines (BV-2 or 6-3) to examine the impact of LS. The mRNA expression of Nos2, an enzyme that catalyzes and modifies the synthesis of NO a substance crucial for inflammation and neurotransmission regulation was found to be decreased by a 36 mmol/L drop in sodium content.
This was further supported by studies carried out under LS settings when researchers observed that microglial cells produced less NO. Furthermore, the nuclear factor of activated T cells-5 (NFAT5), a protein that controls the expression of genes related to osmotic stress, was also decreased by LS. Additionally, in BV-2 cells, overexpression of NFAT5 markedly raised NO generation and Nos2 mRNA expression.
Moreover, the researchers saw a notable increase in NO generation when these microglial cell lines were subjected to quick correction of low salt concentrations. This implies that the abrupt rise in Nos2 mRNA expression and, consequently, NO release, which results in ODS pathogenesis, is facilitated by the quick correction of hyponatremia.
The researchers also found that in microglia isolated from the cerebral cortex of chronic hyponatremia model mice, the expressions of Nos2 and Nfat5 mRNA were decreased.
In conclusion, these results document the effects of persistent hyponatremia and its prompt correction on microglia, hence indicating its role in hyponatremia-induced neuronal dysfunctions.
Clarifying the effect of chronic hyponatremia on brain functions can contribute to the development of new therapeutics and technology to address this condition, while also lowering the occurrence of associated complications and improving the quality of life of patients.”
Yoshihisa Sugimura, Professor, School of Medicine, Fujita Health University
Source:
Journal reference:
Fujisawa, H., et al. (2024) Prolonged extracellular low sodium concentrations and subsequent rapid correction modulate nitric oxide production dependent on NFAT5 in microglia. Free Radical Biology and Medicine. doi.org/10.1016/j.freeradbiomed.2024.08.019.