Satellite cells are muscle stem cells responsible for muscle growth and regeneration in the postnatal stages. While these cells could significantly improve the success rates of experimental cell therapies in treating skeletal muscle conditions, they are rare and found only in small quantities in skeletal muscles.
In a recent study published in Nature Biotechnology, a team of researchers used skeletal muscle tissue to obtain in vitro-derived satellite cells or idSCs. They then transplanted the idSCs into murine models to examine their ability to self-renew and regenerate muscle tissue.
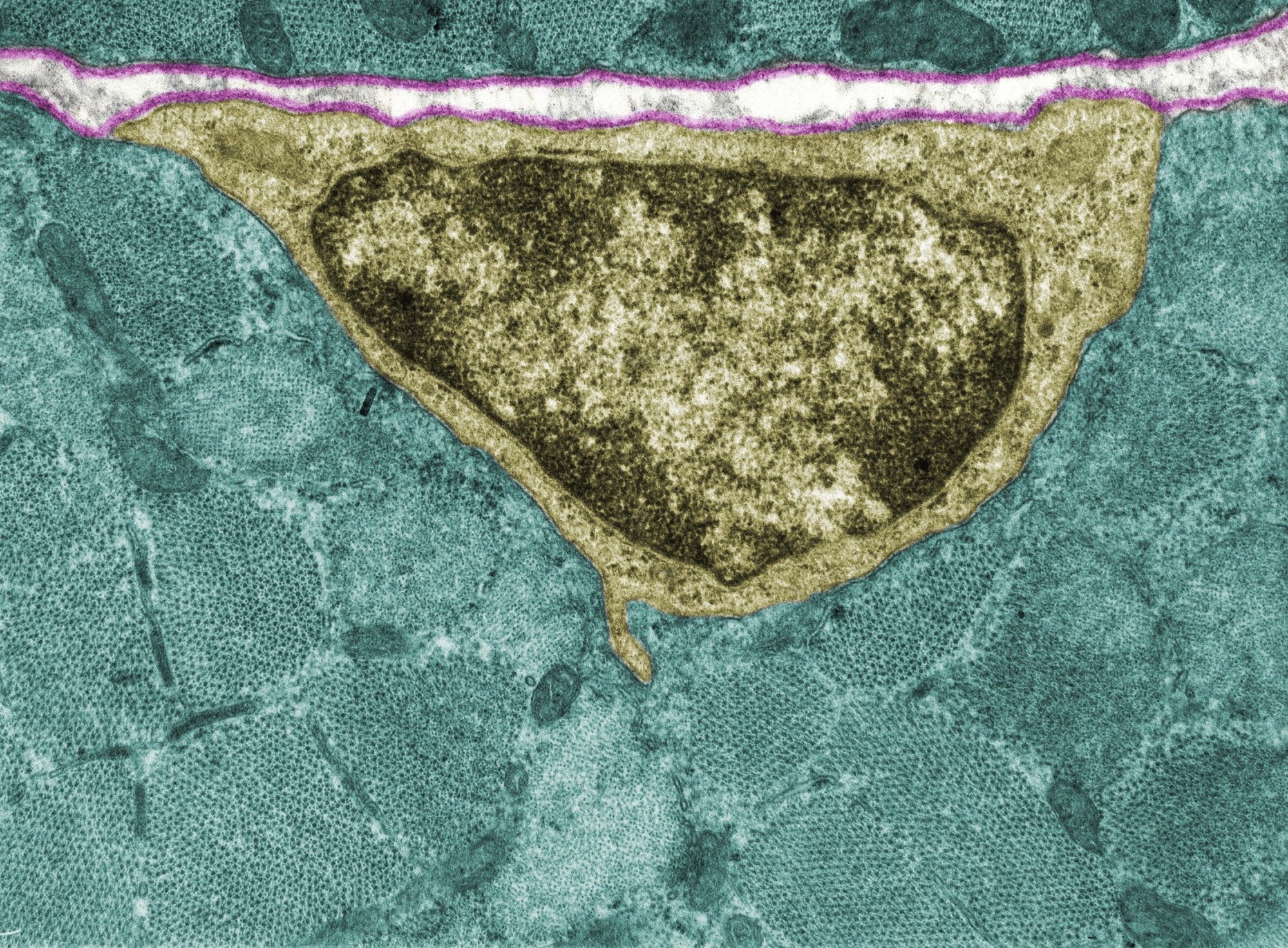 Study: Organoid culture promotes dedifferentiation of mouse myoblasts into stem cells capable of complete muscle regeneration. Image Credit: Jose Luis Calvo/Shutterstock.com
Study: Organoid culture promotes dedifferentiation of mouse myoblasts into stem cells capable of complete muscle regeneration. Image Credit: Jose Luis Calvo/Shutterstock.com
Background
Satellite cells exist in an inactive state in the body and get activated during muscle repair. When activated, satellite cells either self-renew or form myoblasts that further develop into muscle fibers. Muscle regeneration is dependent on satellite cells.
Although the idea of using satellite cells for treating diseases associated with the muscular system is promising, the limited number of satellite cells present in the muscle tissues has prevented stem cell therapies using skeletal cells from progressing further.
Furthermore, culturing skeletal cells has proven difficult because, in culture media, skeletal cells mature into myoblasts, which are less effective after transplantation for long-term regeneration of muscle fiber.
However, recent advances in the development of organoids and induced pluripotent stem cells from adult cells have shown that culturing cells in three-dimensional environments that mimic natural conditions allows stem cells to retain their regenerative state.
About the Study
The present study employed murine models, cell cultures, and various molecular biology techniques to derive idSCs from skeletal muscle tissue and examine its ability to self-renew and proliferate.
Numerous genetically modified mouse models were used for the analysis. Myoblasts and satellite cells were isolated from the skeletal muscle tissue of mice. These cells were then digested using collagenase and dispase and cultured or used directly.
Fluorescence-activated cell sorting was used to purify the myoblasts obtained from the muscle tissue. The myoblasts were also cultured in different media to obtain reserve cells and differentiated myoblasts.
The cultured myoblasts were seeded into spinner flasks and grown under specific conditions to obtain mouse skeletal muscle organoids. Additionally, human myoblasts were also used to obtain human skeletal muscle organoids.
Subsequently, the researchers infected the myoblasts with lentiviral vectors expressing the red fluorescent protein tdTomato and luciferase to enable cell tracking.
The cells that were infected were selected for enrichment. The expression of nestin-green fluorescent protein and other antibodies was also used as a basis for cell sorting and selection for culturing or direct use.
The satellite cells, induced satellite cells, and myoblasts were then transplanted into mice with damaged tibialis anterior muscles to observe engraftment and muscle regeneration. Bioluminescence imaging was used to measure the transplantation efficiency.
The researchers electrically stimulated the transplanted muscle to measure the in situ muscle force and recorded the generated muscle force. A wide range of molecular methods, such as ribonucleic acid (RNA) extraction, quantitative polymerase chain reaction (qPCR), RNA sequencing, and assay for transposase-accessible chromatin with sequencing (ATAC-seq) were used to study gene expression and chromatin assembly in the transplanted muscle.
Major Findings
The study found that although initially, the cultured myoblasts expressed both the transcription factors, MyoD and Pax7, that are involved in muscle differentiation, after 30 days, the expression levels of MyoD decreased and Pax7 increased, indicating a shift towards the satellite cell stage.
These induced satellite cells exhibited the characteristics of satellite cells, such as inactivity or dormancy, reduced size, and ability to form copies or self-renew.
The RNA sequence profiles also showed similarities between the idSCs and satellite cells, such as upregulated expression of extracellular matrix genes and Notch signaling. However, the idSCs also retained some of the metabolic pathways observed in myoblasts.
The idSCs were also observed to undergo chromatin remodeling, indicating that the progressive adoption of various satellite cell characteristics made them ideal candidates for research on muscle regeneration.
The transplantation experiments using mice also indicated that the idSCs showed better integration and persistence into regenerating muscles than myoblasts. The muscles that were transplanted with idSCs showed significantly better cell engraftment than myoblasts at 21 days.
Furthermore, the muscle tissue transplanted with idSCs generated more muscle fibers than those transplanted with myoblasts. Additionally, idSCs were also able to repopulate the stem cell niche in the tissue, contributing to long-term muscle repair.
Induced re-injury of the muscles resulted in the idSCs exhibiting enhanced regenerative capacity by forming new myofibers and restoring muscle function, similar to the abilities exhibited by satellite cells.
In fact, in one of the mouse models for muscular dystrophy, the performance of idSCs surpassed that of freshly isolated satellite cells in engraftment as well as niche repopulation.
Conclusions
In summary, the study demonstrated that induced satellite cells derived from myoblasts exhibit self-renewal and regenerative capabilities similar to that of satellite cells.
Furthermore, the idSCs were able to engraft successfully, occupy the stem cell niche, proliferate, and restore muscle function in mouse models of muscle injury.
The ability of idSCs to persist in the stem cell niche and regenerate muscle tissue in the long term makes them an ideal candidate for muscle repair therapies in cases of muscle damage or muscular degenerative diseases.
Journal reference:
-
Price, F. D., Matyas, M. N., Gehrke, A. R., Chen, W., Wolin, E. A., Holton, K. M., Gibbs, R. M., Lee, A., Singu, Pooja S, Sakakeeny, J. S., Poteracki, J. M., Goune, K., Pfeiffer, I. T., Boswell, S. A., Sorger, P. K., Srivastava, M., Pfaff, K. L., Gussoni, E., Buchanan, S. M., & Rubin, L. L. (2024). Organoid culture promotes dedifferentiation of mouse myoblasts into stem cells capable of complete muscle regeneration. Nature Biotechnology. doi:10.1038/s41587024023447. https://www.nature.com/articles/s41587-024-02344-7