Reviewed by Danielle Ellis, B.Sc.Sep 25 2024
In the UK’s largest study to date, novel steps have been taken to gain a better understanding of the immediate and long-term effects of COVID-19 on the brain.
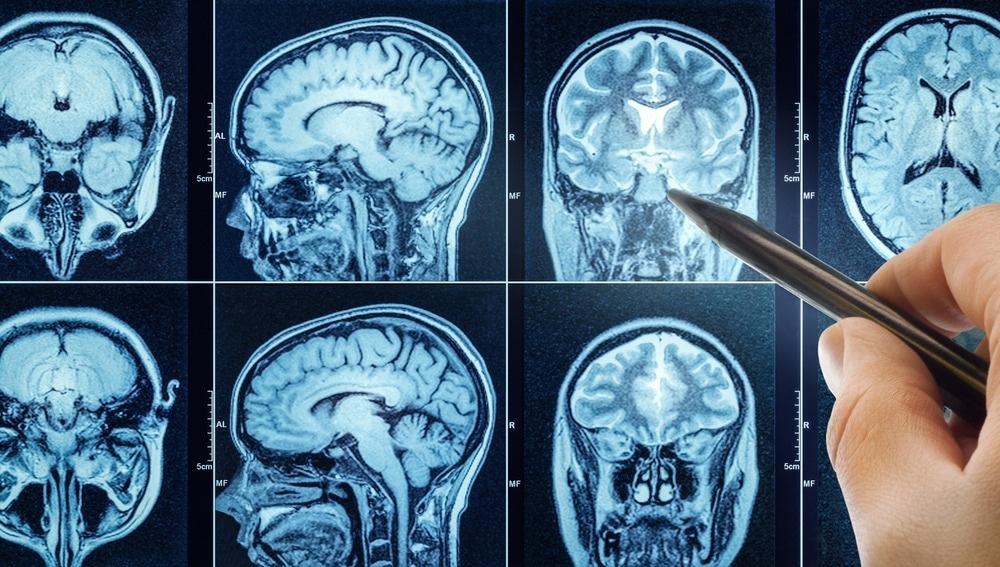
Image Credit: Triff/Shutterstock.com
The study, published in Nature Medicine, was led by researchers from the University of Liverpool, King’s College London, and the University of Cambridge as part of the COVID-CNS Consortium. It found that 12–18 months after hospitalization for COVID-19, patients had worse cognitive function than matched controls.
Significantly, these results are associated with abnormally elevated blood levels of brain injury proteins and decreased brain volume in specific regions on MRI scans.
Remarkably, the study’s findings of post-COVID cognitive deficits were comparable to twenty years of typical aging. It is imperative to underscore that the patients in question were hospitalized due to COVID-19, and it would be inappropriate to extrapolate these findings to the entire population of individuals who have experienced COVID-19.
Nonetheless, the extent of the deficit in every cognitive skill examined, along with the connections to brain damage found in blood and brain scans, offer the most convincing proof to date that COVID can still have a major effect on mental and cognitive health even after recovery from respiratory issues.
The study is part of the University of Liverpool's COVID-19 Clinical Neuroscience Study (COVID-CNS), which aims to investigate further the biological causes and long-term consequences of neurological and neuropsychiatric challenges in hospitalized COVID-19 patients.
After hospitalization with COVID-19 many people report ongoing cognitive symptoms often termed ‘brain fog.’ However, it has been unclear as to whether there is objective evidence of cognitive impairment and, if so, is there any biological evidence of brain injury; and most importantly if patients recover over time.”
Dr. Greta Wood, Study Author and Academic Clinical Fellow - Infectious Diseases, University of Liverpool
Dr. Wood added, “In this latest research, we studied 351 COVID-19 patients who required hospitalization with and without new neurological complications. We found that both those with and without acute neurological complications of COVID-19 had worse cognition than would be expected for their age, sex, and level of education, based on 3,000 control subjects.”
Corresponding author Professor Benedict Michael, Professor of Neuroscience at the University of Liverpool added, “COVID-19 is not a condition simply of the lung. Often those patients who are most severely affected are the ones who have brain complications. These findings indicate that hospitalization with COVID-19 can lead to global, objectively measurable cognitive deficits that can be identified even 12-18 months after hospitalization.”
He added, “These persistent cognitive deficits were present in those hospitalized both with and without clinical neurological complications, indicating that COVID-19 alone can cause cognitive impairment without a neurological diagnosis having been made. The association with brain cell injury biomarkers in blood and reduced volume of brain regions on MRI indicates that there may be measurable biological mechanisms underpinning this.”
“Now our group is working to understand whether the mechanisms that we have identified in COVID-19 may also be responsible for similar findings in other severe infections, such as influenza,” he further stated.
Professor Gerome Breen from King’s College London added, “Long term research is now vital to determine how these patients recover or who might worsen and to establish if this in unique to COVID-19 or a common brain injury with other infections. Significantly our work can help guide the development of both similar studies in those with Long-COVID who often have much milder respiratory symptoms and also report cognitive symptoms such as ‘brain fog’ and also to develop therapeutic strategies.”
More About COVID-CNS
The COVID-19 Clinical Neuroscience Study (COVID-CNS) is a £2.3 million UKRI study led by researchers from the University of Liverpool and King's College London. COVID-19 causes acute neurological and neuropsychiatric complications in 20-30% of hospitalized patients.
Researchers are investigating the acute neurological and neuropsychiatric effects of infection, as well as the long-term clinical and cognitive outcomes, with the goal of determining the underlying biological processes driving these effects through a better understanding of brain injury, immune responses, and genetic risk factors.
Source:
Journal reference:
Wood, G. K., et. al. (2024) Post-hospitalisation COVID-19 cognitive deficits at one year are global and associated with elevated brain injury markers and grey matter volume reduction. Nature Medicine. doi.org/10.1038/s41591-024-03309-8