Drug development faces many hurdles from discovery to clinical trials. An example of such a hurdle is through drug delivery. Drug delivery is the process of transporting a given drug into or within the body to its target tissue or cell, it is a vital aspect of the success of novel treatment options.
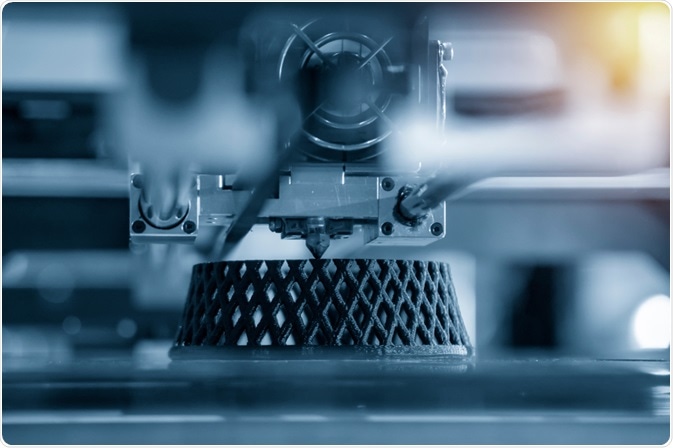
3D Printing. Image Credit: Pixel B/Shutterstock.com
The efficacy of a drug (the maximum achievable response) can be impacted by the method of drug delivery. To address such problems, novel solutions can be found in existing techniques.
3D printing (3DP) technology has been repurposed to apply to pharmaceutical development, in recent years it has been used to produce tablets of personalized dosage and combine several prescriptions into one tablet. Future possible developments discuss methods of sustained release and the ability to integrate into sites of injury or trauma specifically to assist the healing process.
3D Bioprinting in History
First discovered and developed in the 1980s, 3DP is a relatively novel tool in the medical field. The first medical application of 3DP was in the early 2000s for the production of custom dental prostheses. From then, 3DP was seen as an inexpensive alternative means of producing custom prosthetic limbs and less common prostheses such as windpipes.
Then came the advent of bioprinting functional organs. The creation of “Bio-Ink”, a polymer gel scaffold containing cells of specified origin with the potential to print fully artificial organs. In 1988, an inkjet printer was used to deposit cells in a pattern labeled “cyto-scribing” marking the first recorded use of bio-printing.
In 2001, cyto-scribe technology was used to seed patient-sourced cells into a bladder-shaped scaffold which was later implanted with no adverse impact. The first fully printed functional organ was a miniature kidney in 2003.
3DP for drug delivery is a newer concept, historically 3DP has been used to recreate diseased tissue in which specific methods of delivery can be tested, one such example is the reconstruction of a fetal airway to test aerosol drug delivery to the lungs. Recently 3DP has been utilized to produce drugs themselves.
The pharmacy of the future? Personalized pills, 3D printed at home | Daniel Kraft
The First 3DP Drug on the Market
The first 3DP drug was approved for usage in 2015. Used for treating epilepsy, specifically partial-onset seizures in children of 4 years, myoclonic seizures in ages 12 and over with juvenile myoclonic epilepsy, and primary generalized tonic-clonic seizures in ages 6 and older.
The manufacturer of the drug copyrighted its technology to develop the porous and rapidly disintegrating structure. This technology simplifies ink formation and allows the production of high-dose medicines. This method allows for rapid scaled-up production, but it is difficult to use to personalize medicine and combine drugs due to the different powdered ingredients needed to be layered precisely between print passes. The benefits of such a tablet are the ease of administration by self or carer, the high dosage ability of one tablet, and the rapid mode of action.
Combining Medication into an Easy-To-Swallow Pill
The act of combining several drugs into one pill is not a novel idea, but one that is facilitated by the use of 3DP. The commercially available polypill called “Polycap” is a five-in-one dosage for the prevention of cardiovascular events and stroke.
A 2015 study managed to combine the same 5 drugs and observed their sustained release profiles by using 3DP. These drugs were physically separated using cellulose-based materials. Though, there are issues with which drugs can be combined into polypills, such as those that are susceptible to heat-induced degradation as they cannot withstand the >200°C heat-based deposition of a 3D printer. There were few reports of a pill with a single drug formulation with multiple release mechanisms at the time of this study. Other notable issues involved ink bleeding and migration as a result of printing larger doses.
Within the aforementioned study, the issue is with comorbidities in patients over 55 who experience cardiovascular and renal complications who can have several necessary medications would most benefit from a combined pill. The polypill studied successfully delivered 5 different drugs via 2 release mechanisms, sustained and immediate. Drugs were physically separated within the pill and no detectable interaction and thus could be a convenient remedy to promote treatment adherence in patients.
Stereo-Lithography
Most of the previous techniques make use of fused deposition modeling (FDM), stereolithography (SLA) is a novel 3D printing method that can be used to develop multiple layers with variable drug content and shape. With this development polypills can provide more personalized drug combinations for ease of consumption, the freedom to combine different drugs is made possible by 3DP allowing printing of different geometrical structures to alter release rate, size of molecules and differing material also assist in the altered release.
One positive is through SLA, thermal degradation is avoided, the resolution is improved, the accuracy is greater, and production is much faster. In 2019, the limitation of SLA printing polypills was overcome through the development of a new printer capable of printing multi-layered tablets.
The development of a new machine increased SLA capability to tailor polypills which contain up to 6 active ingredients. Most importantly, this study displayed the capability of polypill development using this method.
Conclusion
From its advent, 3DP was a game-changing technology that revolutionized several different industries. Its impact on drug production and delivery has eased the development of easy to administer and easy to swallow pills. Though there is only one 3DP drug on the market, there is every possibility for more to be developed in the near future.
Sources:
- Ventola, C Lee. “Medical Applications for 3D Printing: Current and Projected Uses.” P & T: a peer-reviewed journal for formulary management vol. 39,10 (2014): 704-11.
- Zeming Gu, Jianzhong Fu, Hui Lin, Yong He, Development of 3D bioprinting: From printing methods to biomedical applications, Asian Journal of Pharmaceutical Sciences, Volume 15, Issue 5, 2020, Pages 529-557, ISSN 1818-0876, https://doi.org/10.1016/j.ajps.2019.11.003.
- Wake Forest School of Medicine. (n.d.). A Record of Firsts. [online] Available at: https://school.wakehealth.edu/Research/Institutes-and-Centers/Wake-Forest-Institute-for-Regenerative-Medicine/Research/A-Record-of-Firsts [Accessed 14 Jan. 2021].
- Wen-Kai Hsiao, Barbara Lorber, Herbert Reitsamer & Johannes Khinast (2018) 3D printing of oral drugs: a new reality or hype?, Expert Opinion on Drug Delivery, 15:1, 1-4, DOI: 10.1080/17425247.2017.1371698
- Khaled, S., Burley, J., Alexander, M., Yang, J. and Roberts, C., 2015. 3D printing of five-in-one dose combination polypill with defined immediate and sustained release profiles. Journal of Controlled Release, 217, pp.308-314.
- Robles-Martinez, P.; Xu, X.; Trenfield, S.J.; Awad, A.; Goyanes, A.; Telford, R.; Basit, A.W.; Gaisford, S. 3D Printing of a Multi-Layered Polypill Containing Six Drugs Using a Novel Stereolithographic Method. Pharmaceutics 2019, 11, 274. https://doi.org/10.3390/pharmaceutics11060274
Further Reading