The intrusion of any foreign material inside the human body triggers the immune system. The immune system provides protection against bacteria, viruses, and also gets activated after artificial implantations. Biomaterial implantation is associated with surgical procedure, which causes injury to a tissue or organ.
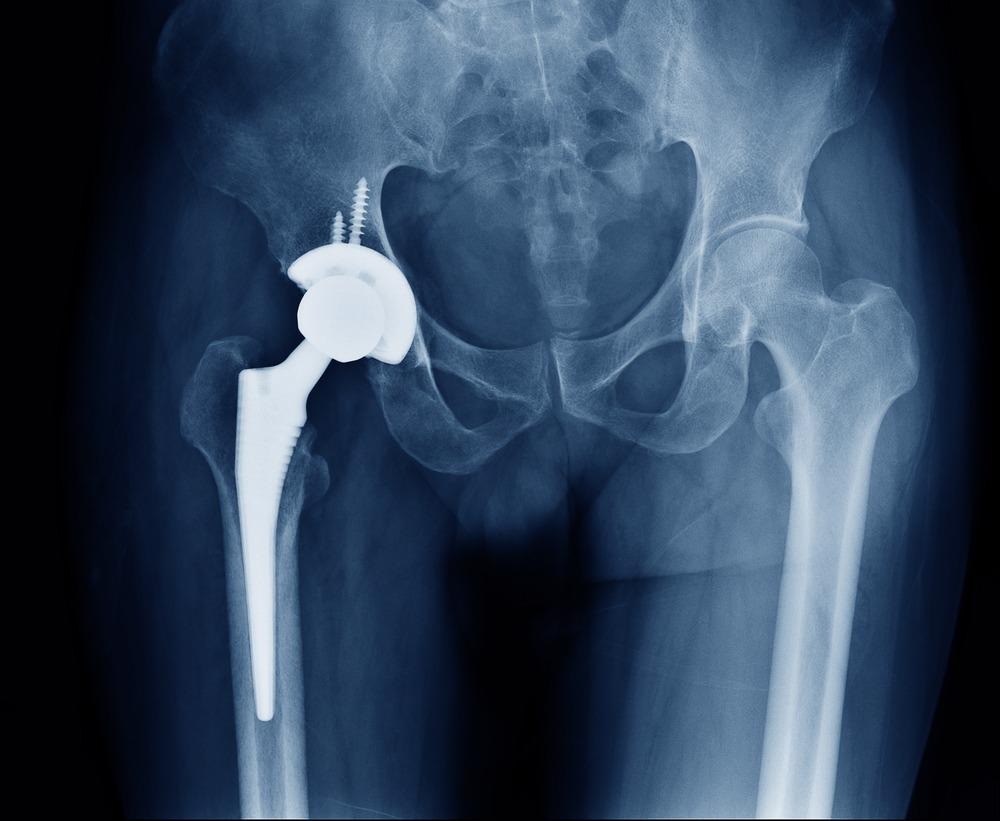
Image Credit: ChooChin/Shutterstock.com
Research revealed that all implants trigger immune reactions, and 35% of individuals with implants require a secondary operation to replace it owing to such reactions. The immune response induced by artificial implants could be managed via immunodepressant therapy.
Implantation of engineered cell material induces adaptive immune response towards the cellular component and, thereby, dysregulates the host response to the material component. Similarly, in the case of biodegradable devices, the immune response could be triggered by the degradation products and surface changes of the biomaterial caused after the process of degradation. This article focuses on the immune response to implants.
Implants and Immune Responses
As early as nanoseconds after implantation, the tissues, proteins from blood, and intestinal fluids are adsorbed to the surface of the biomaterial. This causes the activation of the complement system, coagulation cascade, platelets, and immune cells. It also promotes the formation of a transient provisional matrix and triggers an inflammatory response. Inflammatory responses play a vital role in immunity.
Blood coagulation on biomaterials requires the combination of both contact activation and platelet adhesion. Implants trigger factor XII (FXII) and tissue factor (TF) that are associated with the activation of the coagulation cascade. TF initiates leukocytes at the implantation site and activates biomaterial attached platelets. FXII also stimulates the generation of thrombin, one of the main activators of platelets. Thrombin induces the cleavage of fibrinogen to fibrin and, thereby, develops a primary fibrous mesh around the biomaterial.
Upon contact with implants, complement pathways get activated. In the case of inflammation, complement activation occurs via three distinct pathways, namely, the alternative, the classical, and the lectin pathway. These pathways are based on the level of C3 convertase activation, which facilitates the formation and release of the anaphylatoxins C3a and C5a. Activation of the complement system is related to biomaterials adsorbed protein layer.
After initiation of the complement cascade, high concentrations of C3a and C5a are released at the implantation site. Anaphylatoxins (complement peptides) are produced upon activation of the complement system that influences the onset of inflammation in the implantation site. This peptide has a multitude of effector functions that include triggering mast cell degranulation, attracting and activating granulocytes and monocytes, increasing vascular permeability, and inducing the release of granulocyte ROS (reactive oxygen species).
Integrins are transmembrane receptor proteins that mediate adhesion during biomaterial-associated macrophage fusion. Clustering of integrins promotes degranulation, motility, phagocytosis, and release of ROS and cytokines. These events play a crucial role in the inflammatory response toward biomaterials.
Although danger signals or alarmins were not considered as potential activators of leukocytes following biomaterial implantation, several studies have recently revealed that these are capable of activating immune cells at biomaterial surfaces. Alarmins are recognized by cells of the innate immune system, e.g., macrophages and dendritic cells (DCs) through pattern recognition receptors (PRR), which promote inflammation and immunity. Therefore, biomaterial-associated alarmins could interact with PPRs (e.g., TLRs on leukocytes) and promote inflammation.
Chronic inflammation occurs when inflammatory stimuli persist at the implant site with macrophages causing prolonged immune responses. The monocytes undergo a phenotypic change differentiating to macrophages at the implantation site, resulting in further dissemination of chemoattractants. Macrophages bound to the implant biomaterials can nurture the attack of additional inflammatory cells by producing chemokines like IL-8, MCP-1, MIP-1b.
Although synthetic biomaterials (e.g., ceramics, polymers, or metallic materials) are known to be non-immunogenic, lymphocytes have been found at Implantation sites, indicating their involvement in immune responses. Dendritic cells induce adaptive immune responses and possess immunoregulatory capacities.
Matrix metalloproteinases (MMPs) are macrophage-derived proteolytic enzymes, which are associated with the foreign body reaction to biomaterials. Among MMPs, an increased level of MMP-9 indicates inflammation and is also associated with poor wound healing.
Modification in the Surface Topography of the Breast Implants Positively Influenced Immune Responses
Approximately, 400,000 people receive silicone breast implants each year in the United States. The majority of the implants are required to be replaced within 10 years due to various complications, including the generation of scar tissue.
Recently, a group of researchers at MIT have systematically analyzed how the different surface architectures found on these implants trigger adverse effects, including the development of an unusual type of lymphoma (rare cases). The surface topography of the implants affects the immune response. This is the reason why scientists investigated the impact of various degrees of surface roughness (from smooth to high texture) of silicone breast implants on the immune system and the surrounding tissue.
Researchers performed experiments on the rabbit model and revealed that tissue exposed to the roughest implant surfaces had shown increased activity from macrophages, whose primary function is to eliminate foreign cells and debris. Also, these implants induced more pro-inflammatory T-cell responses and more scar formation.
Scientists inferred that rougher implants rub against the surrounding tissue and cause more irritation. This might be the reason why rougher implants can lead to lymphoma. Smooth surface implants also induce higher levels of macrophage response and fibrosis.
However, interestingly, implants with altered surface topography with 4-micron average roughness were found to trigger T cells that suppressed tissue inflammation. Therefore, implants with the optimal surface architecture, including surface roughness at about 4 microns on average, could significantly reduce the amount of scarring and inflammation compared to other types of surfaces.
Further Reading
Last Updated: Dec 17, 2021