Scientific research in the past century has shed light on the role of the crosstalk between tumor and tumor microenvironment in the disease outcome of cancer. This has led to the development of various therapeutic strategies to exploit this relationship to eliminate the progression of cancer.
In fact, the Nobel prize for medicine 2018 was awarded to the discovery of exploiting negative immune regulation of T cells as a powerful anti-cancer strategy.
Immunosurveillance
Cancer is a genetic disease that is characterized by the abnormal and uncontrolled division of specific cells. The constant pursuit of immune cells to identify and neutralize the tumor cells is called immunosurveillance. Despite the many efforts of the immune response to monitor and eliminate cancer cells, cancer cells evolve genetically to evade the immune response and continue to survive and divide, resulting in tumor growth.
Some of the key players in immunosurveillance are dendritic cells, natural killer cells, cytotoxic T cells, and Helper T cells. Natural killer cells sense stress-associated molecules on cancer cells and destroy them. Helper T cells produce cytokines such as interleukins and interferon-gamma (IFNg), which are used to recruit more natural killer cells to the tumor site. Helper T cells also assist dendritic cells to activate cytotoxic T cells.
Dendritic cells identify tumor-specific antigens present on the tumor cells and present them to the cytotoxic T cells. Cytotoxic T cells bind to the tumor cells and release perforins and granzymes into the tumor cells to destroy them. This well-coordinated effort by the immune cells is crucial for killing cancer cells.
Mechanisms used by tumor cells to evade immune response
During the cancer growth, some of the cancer cells that were not killed by the immune cells will undergo genetic transformation offering the tumor heterogeneity, which means the tumor will comprise cancer cells with different genetic make-up.
While the immune cells continue to kill the cancer cells, the genetic make-up of some of the cancer cells in the tumor will offer an advantage of being unrecognizable by the body’s immune system and these cells will eventually outgrow the rest of the cancer cells. This phenomenon is called immunoediting. Another way cancer cells evade the immune system is by expressing molecules called immune checkpoints that suppress the immune system. Immune checkpoints such as PDL-1 and CTL4 binds to the receptors on the T cells and inactivate them. Lastly, tumor cells may express molecules that can attract immune cells such as regulatory T cells and other myeloid cells that facilitate tumor growth.
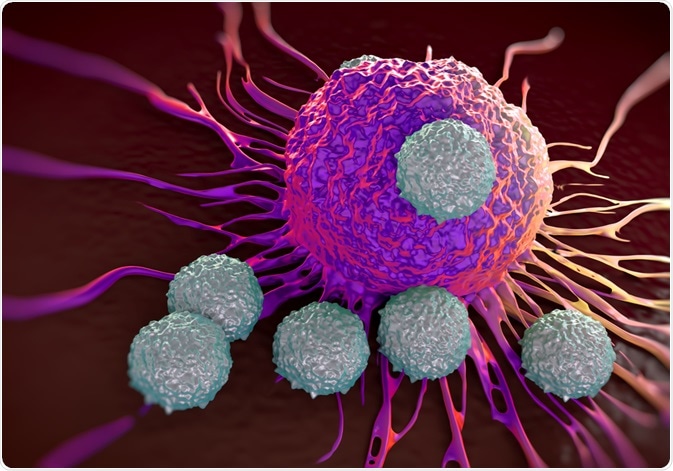
Image Credit: Peddalanka Ramesh Babu/Shutterstock.com
Immunotherapy
The idea of using the body’s own immune system was first studied by William Coley in 1893. After observing tumor regression in a streptococcus infected patient, Coley tested the hypothesis that cancer can be treated by stimulating the immune system. He injected a mixture of bacteria and bacterial products (Coley’s toxin) in several patients and saw regression of cancers as a result of the immune response of the body to the bacteria.
The field of immunotherapy is breaking new ground in recent decades. Various therapeutic strategies are now being used and tested to treat cancer, including non-specific immune stimulation, adaptive cell transfer, immune checkpoint blockade, and vaccination strategies. The Non-specific immune stimulation aims to provide a general boost to the immune cells.
Cytokines such as IL-2 and IFNg are approved for use in the treatment of melanoma. Bacterial tuberculosis vaccine, Bacille Calmette-Guerin (BCG) is currently being used to treat early-stage bladder cancer. Immune checkpoint inhibitors such as Ipilumimab binds to the checkpoints such as CTLA4 and inhibit the binding of checkpoints to the receptors on the T cells, therefore, allowing the cytotoxic T cells to destroy the cancer cells.
Adaptive cell transfer involves isolating a patient’s specific immune cells invading the tumor, growing them in cell culture, and transferring the most effective T cells into the patient to kill the tumor cells. Genetically engineered viral vaccines obtained from viruses such as the Herpes simplex virus are being currently developed to treat melanoma, head and neck cancer.
Conclusion
The effectiveness of immune checkpoint inhibitors and other drugs that employ the body’s immune system to treat cancer suggests that immunotherapy is an effective strategy to battle cancer. However, immune checkpoint inhibitors currently available are only effective in a limited percentage of cancer patients.
Therefore, there is a need for a better understanding of tumor immunology at a deeper level. On the Brightside, the combination of immunotherapy with chemotherapy and radiation seems to be promising in clinical trials.
Sources:
- Galon, J & Bruni, D. Tumor Immunology and Tumor Evolution: Intertwined Histories, Immunity reviews, 52, 55-81(2020). doi: 10.1016/j.immuni.2019.12.018.
- Sogn, J. A. Tumor Immunology The Glass Half Full. Immunity reviews, 9,6, P757-763 (1998). doi: https://doi.org/10.1016/S1074-7613(00)80641-X
- Waldman, A.D., Fritz, J.M. & Lenardo, M.J. A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat Rev Immunol 20, 651–668 (2020). Doi: https://doi.org/10.1038/s41577-020-0306-5
Further Reading