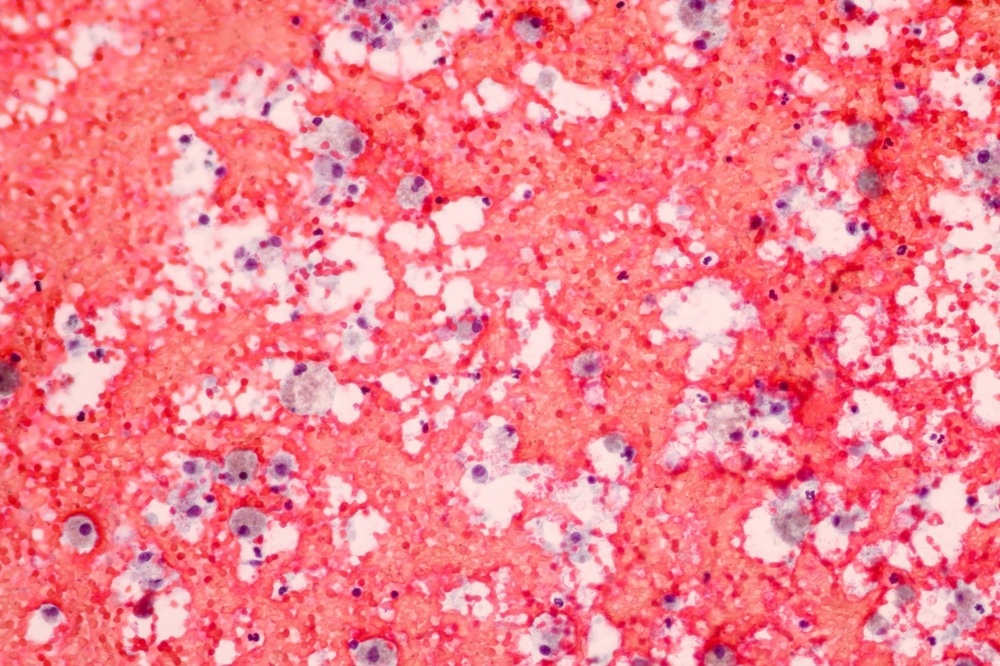
Macrophages are innate immune cells that fulfill various roles within the immune system. They are relatively large leukocytes, at around 20 µm diameter, and have spherical nuclei. They are a crucial component of microbial immunity, tissue healing, and repair, as well as being implicated in some pathological conditions, such as suppression of tumor immunity and autoimmunity.
 Immunology?" />
Immunology?" />
Image Credit: Komsan Loonprom/Shutterstock.com
There is a spectrum of phenotypes that macrophages can express, ranging from pro-inflammatory to anti-inflammatory poles, typically characterized by their expression of specific antigens and cytokines. This article will provide an overview of the development and some of the functions of macrophages.
Macrophage Development
Macrophages are an active, differentiated form of monocytes, which evolve from myeloid progenitors in the bone marrow and migrate to the circulatory system and peripheral tissues. Monocytes can also differentiate into dendritic cells, which have other roles in immunity and tissue development, and the fate of these monocytes is directly linked to heterogeneity in their phenotypes and the cytokine signals they receive from the tissues they are localized in.
Differentiation to pro-inflammatory, or M1-like, macrophages is driven primarily by interferon-gamma, a cytokine produced by T cells, natural killer cells, and mature macrophages. At the other end of the spectrum, differentiation into anti-inflammatory, or M2-like, macrophages are induced by a range of interleukin cytokines and the growth factor ‘macrophage colony-stimulating factor’.
Macrophages are defined not only by their phenotype but also by their localization, leading to nervous system macrophage sub-types being known as microglial cells and bone-specific ones being referred to as osteoclasts. It has also emerged relatively recently that many tissue-resident macrophages do not evolve from monocytes following stimulation but were, in fact, seeded during the embryonic stage of development.
Microbial Immunity and Phagocytosis
As their name suggests, phagocytosis, or ‘eating’ of cells and cell debris, is one of the primary functions of macrophages. This is key in recognizing microbial infections, and macrophages can engulf a variety of pathogens and pathogen particles, including primarily those that have been opsonized, or ‘tagged’, by the adaptive immune system or the complement system.
Macrophages that have migrated to infected tissue due to cytokine release and recognition of pathogen-associated molecular patterns will engulf infectious material and process it to then be presented to adaptive immune cells to facilitate a more specific immune response and subsequent infection clearance.
Antigen Presentation
Macrophages, specifically those with more M1-like phenotypes, are efficient antigen-presenting cells (APCs). Once they have engulfed infectious material, including intracellular or extracellular pathogens, viral particles, or excreted toxins, they process it into sections with recognizable epitopes.
These sections, or antigens, are then presented extracellularly, alongside major histocompatibility complex (MHC) and co-ligands, to lymphocytes in secondary immune tissues. These lymphocytes then initiate an adaptive immune response, including the production of antigen-specific antibodies and opsonization of pathogens for easier recognition and disposal.
Tissue Repair
Macrophages not only phagocytose infectious material but also apoptosed cells and host cell debris to clear damaged tissue and allow for repair following damage by infection or injury. M2-like polarised macrophages also aid tissue repair by clearing inflammatory signals and releasing anti-inflammatory cytokines such as interleukin 10. It has also been shown that M2-like macrophages can inhibit apoptosis to further reduce tissue damage via the release of the protein ‘apoptosis inhibitor of macrophage’.
In addition to this, M2-like macrophages also secrete growth factors, promoting cell growth in previously damaged tissues and initiating the process of repair.
Tumour Immunity
Tumor-associated macrophages (TAMs) are abnormal macrophages that influence tumor growth, via complex regulation mechanisms. These pathways involve TAM cytokine expression, including suppression of T cell differentiation via expression of programmed cell death ligand 1 (PD-L1), which is a common target in newly-developed immunotherapy treatments, and suppression of CD8+ T cells via the actions of interleukin 10.
Interleukin 10 also promotes the recruitment of regulatory T cells, suppressing other parts of the immune response. In addition to this, TAMs cannot migrate to lymph nodes like normal macrophages ought to, meaning that they are unable to present antigens to lymphocytes and induce an adaptive immune response that way. There are also many other potential immune suppressive pathways of macrophages in tumors that remain understudied. Overall, TAMs have several roles in tumor progression and targeting them as a therapeutic option remains a vital field of study.
Image Credit: peterschreiber.media/Shutterstock.com
Autoimmunity
Macrophages are pathologically involved in other forms of disease progression, not just tumor growth. One example of this is autoimmunity or the pathological action of the immune system against host tissue. Macrophages can contribute to a range of autoimmune diseases through various mechanisms.
One of these is the presentation of auto-antigens to lymphocytes. There are many cellular mechanisms to prevent this from causing disease, such as the requirement for several co-signaling molecules; however, if these act aberrantly, then macrophages can contribute to initiating an adaptive immune response to host antigens. Additionally, the over-expression of pro-inflammatory cytokines in M1-like macrophages can contribute to autoimmune conditions involving significant inflammation, such as rheumatoid arthritis. This can be due to intracellular signaling issues, lack of M2-driving cytokines in the tissue microenvironment, or other failures in the resolution of inflammation.
Overall, macrophages have many roles in immunity and disease due to their range of possible phenotypes.
Sources:
- DeNardo DG, Ruffell B (2019) Macrophages as regulators of tumour immunity and immunotherapy. Nat Rev Immunol 19(6):369–382. https://doi.org/10.1038/s41577-019-0127-6
- Kourtzelis I, Hajishengallis G, Chavakis T (2020) Phagocytosis of Apoptotic Cells in Resolution of Inflammation. Front Immunol 11:553. https://doi.org/10.3389/fimmu.2020.00553
- Shapouri-Moghaddam A, Mohammadian S, Vazini H, Taghadosi M, Esmaeili S-A, Mardani F, Seifi B, Mohammadi A, Afshari JT, Sahebkar A (2018) Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol 233(9):6425–6440. https://doi.org/10.1002/jcp.26429
- Sprangers S, de Vries TJ, Everts V (2016) Monocyte Heterogeneity: Consequences for Monocyte-Derived Immune Cells. J Immunol Res 2016:1475435. https://doi.org/10.1155/2016/1475435
- Zamarron BF, Chen W (2011) Dual roles of immune cells and their factors in cancer development and progression. Int J Biol Sci 7(5):651–658. https://doi.org/10.7150/ijbs.7.651
Further Reading