Immune cells are crucial to regulating the immune response, and a variety of cells each have different responsibilities. This includes all the red blood cells, platelets, and white blood cells, originating from the same progenitor known as hematopoietic stem cells (HSCs).
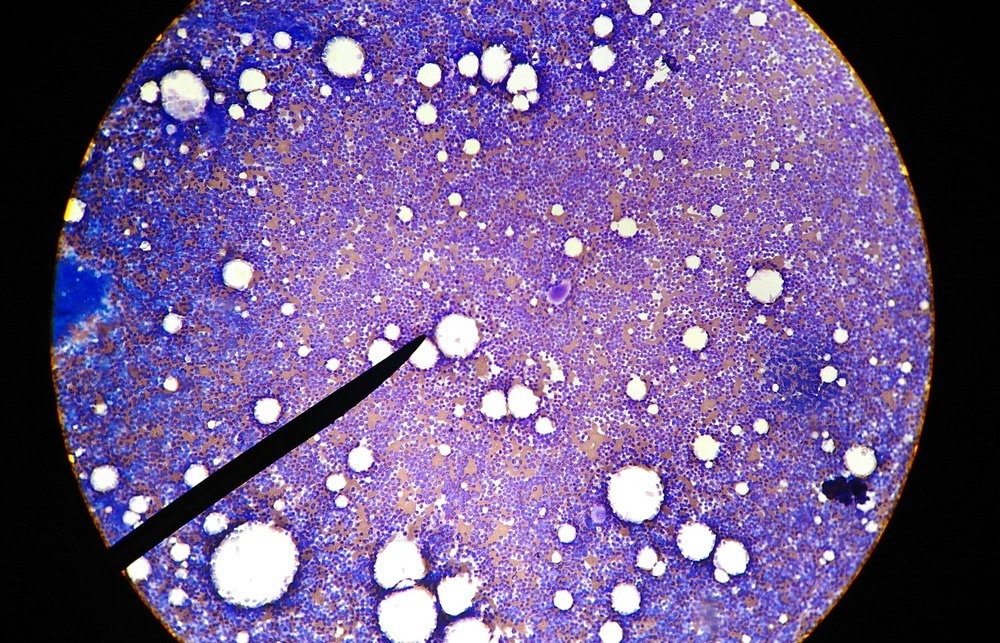
Image Credit: Schira/Shutterstock.com
HSCs can differentiate into various immune cells and have self-renewal properties that play key roles in the immune response. Hence, they are a common choice for transplantation in leukemia, lymphoma, and autoimmune diseases (ADs) patients.
This article will provide an overview of HSCs, the immune cells they give rise to, and their role in the immune response.
Overview of stem cells
HSCs are a group of stem cells (SC) that have undergone a differentiation process. SCs found in both embryos and adult cells and are defined as the unspecialized cells of the body. This means they can differentiate/specialize into any cell type and have self-renewal capabilities.
Specialization consists of different steps, which result in different stem cell types; totipotent SC (TSC), pluripotent SC (PSC), multipotent SC (MSC), oligopotent SC (OSC), and unipotent SC (USC). They all have various differentiation potentials, with TSCs having the highest differentiation potential, i.e., the ability to differentiate into any cell type, such as zygotes. HSCs are known as PSCs due to their ability to differentiate into the progenitors of red blood cells, platelets, and the two categories of white blood cells
White blood cells of the immune system
The white blood cells are derived from two progenitors produced by HSCs. These progenitors are known as myeloid and common lymphoid progenitors. The myeloid progenitor gives rise to immune cells crucial to the immune response. For example, it is a precursor for macrophages, a phagocytic immune cell important in the innate immune response. They circulate in the blood and are responsible for engulfing foreign pathogens.
Another type of immune cell is dendritic cells, which take up the antigen and display it on their surface for lymphocytes to recognize. Among the many immune cells derived from HSCs, neutrophils are phagocytic immune cells responsible for killing extracellular pathogens, making them a primary defense in the innate immune response.
On the other hand, the common lymphoid progenitor produces two types of lymphocytes; the B cells secrete antibodies, and the T cells are differentiated into classes, such as the cytotoxic T cells that kill virus-infected cells and T cells that activate the B lymphocytes.
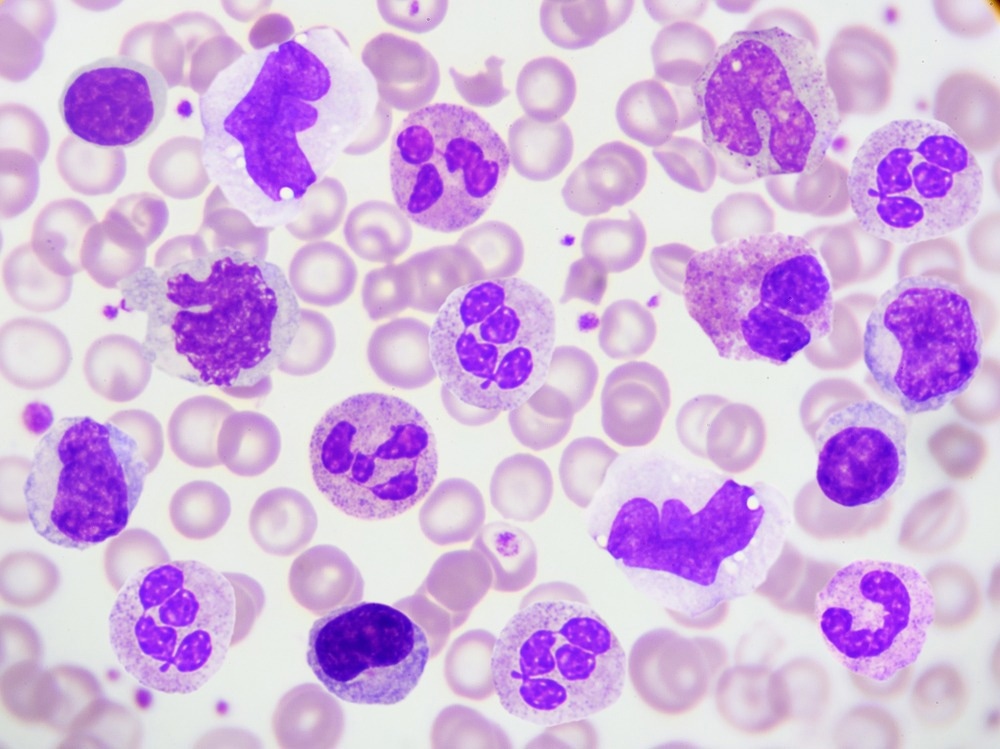
Image Credit: Jarun Ontakrai/Shutterstock.com
HSCs and immune signaling
Research has provided evidence that shows the differentiation and self-renewal properties of HSCs can be altered specifically in response to signals from the immune system and infection. Additionally, the bone marrow microenvironment provides an immune-privileged site for HSCs which means that they are less susceptible to immune responses. HSCs can also suppress innate and adaptive immunity by presenting immune inhibitors allowing stem cells to evade immune surveillance. Furthermore, evidence suggests that HSCs express molecules on their surface that send ‘in’ and ‘out’ signals that communicate with the immune system directly.
For example, the ‘in’ signals are stimulated from infection, which activates HSCs to differentiate into the immune cells mentioned above through toll-like receptors, tumor necrosis factor-alpha, and interferon receptors. The ‘out’ signals are produced by inhibitory molecules such as CD47 and CD274 to inhibit innate and adaptive attacks, giving HSCs ‘immune privilege’. The interaction between these signals determines the differentiation potentials of HSCs and their interaction with the immune system.
HSCs and the immune response
HSCs and the progenitor cell it gives rise to (HSPCs) have a direct role in the host immune response. The immune-privileged site of the HSPCs produces stomal-derived factor-1 (SDF-1), which binds to the receptor CXCR4 to enable HSC self-renewal properties and allow them to remain dormant. When an infection occurs, SDF-1-CXCR4 binding is disrupted, and HSPCs are triggered into differentiating into the myeloid and lymphoid progenitors that produce the white blood cells and lymphocytes to defend against the pathogens. They essentially act as ‘first responders,’ and a plethora of evidence documents the proliferation of HSPCs.
A study demonstrated that when mice were injected with Escherichia coli (E. coli), HSPC proliferation was observed, and similar observations were made with chronic Mycobacterium avian infection. These studies show that the proliferation of HSPCs was part of the primary immune response rather than replacing red blood cells, which is one of their primary roles. Many factors enable HSPCs to respond rapidly to infections, such as pattern recognition receptors (PRRs), which recognize pathogen-associated molecular patterns (PAMPs) presented on the pathogen’s surface.
One of the PRRs expressed by HSPCs is a family of toll-like receptors (TLRs), which are present either on the cell’s surface or intracellularly and recognize membrane components of microbes or viral and bacterial nucleic acids, respectively.
Clinical applications using HSCs
The pluripotent nature of HSCs provides a major potential for their use in transplantation to treat genetic and immune disorders. Studies have demonstrated the origin of cells that make up connective tissue, hepatocytes, cardiac muscle, and lung epithelial cells. This provides a new avenue of treatment that may allow the regeneration of many cell types.
For example, HSC transplantation (HSCT) can treat ADs caused by the development of immune responses toward the body’s cells. So, the transplantation procedure aims to reconfigure the immune system by removing immune system memory resulting in a ‘self-tolerant’ immune system. This procedure allows for treatments to be medication-free, eliminating side effects and the risk of addiction.
Conclusion
To conclude, HSCs are extremely important in regulating the immune response, and alongside the current advents in HSCT combined with further research, it could be a groundbreaking treatment to cure many autoimmune diseases.
Sources:
- Janeway CA Jr, Travers P, Walport M, et al. Immunobiology: The Immune System in Health and Disease. 5th edition. New York: Garland Science; 2001. The components of the immune system. Available from: https://www.ncbi.nlm.nih.gov/books/NBK27092/
- Sahai, J. & Louie, S. G. (1993). ‘Overview of the immune and hematopoietic systems’ Am J Hosp Pharm, 50 (7 Suppl 3), pp. S4-9.
- Zakrzewski, W., Dobrzyński, M., Szymonowicz, M. & Rybak, Z. (2019). ‘Stem cells: Past, present, and future’ Stem Cell Res Ther, 10 (1), p. 68. DOI: 10.1186/s13287-019-1165-5.
- Zhang, C. C. (2012). ‘Hematopoietic stem cells: Interplay with immunity’ Am J Blood Res, 2 (4), pp. 219-27.
Further Reading