Immunological memory can be described as the immune system’s ability to respond to pathogens effectively; this is known as the secondary response, which is stronger than the primary immunological response.
When a foreign antigen is observed in the host more than once, the adaptive immune response is more prepared the second time because memory cells retain the memory of the first encounter with the pathogen. This enables the adaptive immune response to be faster and more effective in fighting against this particular antigen.
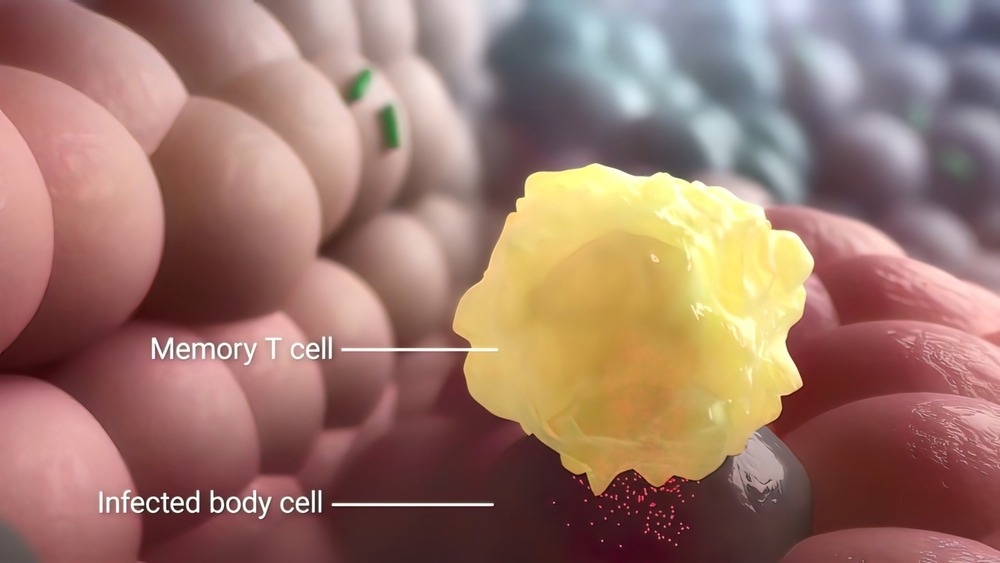
Image Credit: piccreative/Shutterstock.com
Memory Cells in Immunological Memory
This unique property of the immune system to store information about a stimulus or pathogen is significant for protection against bacteria, viruses, and fungi and is also dependent on a subset of cells within T and B lymphocytes and natural killer cells.
T lymphocytes can be divided into T helper cells, cytotoxic T cells, regulatory T cells, and memory T cells. CD4+ memory T lymphocytes have the ability to differentiate from naïve T cells as short-term effector memory cells. CD8+ memory T cells, however, are more linear, with naïve T cells losing their proliferative ability and differentiating into various subsets of T cells such as stem memory T cells, central memory cells, and effector memory T cells.
T cells have T cell receptors (TCRs) and MHC II or I molecules on their surface that aid in triggering T cell activation by antigen-presenting cells (APCs). When T cells are activated, they undergo expansion, contraction, and the initiation of memory cells. This means once the immune response is activated to eliminate a pathogen, the volume of T cells that have been produced is deemed unnecessary, which causes 90-95% of lymphocytes to undergo apoptosis.
The remaining 5-10% of T cells differentiate into memory cells, which can form central memory cells, effector memory cells, tissue-resident memory cells, regulatory T cells, and stem memory T cells.
Different Types of Memory Cells
Central memory T cells can occur in secondary lymphoid organs such as lymph nodes and tonsils. Effector memory T cells, however, can be found in non-lymphoid peripheral tissue such as the lungs, liver, and intestines. These cells can be recirculated between the blood and tissue.
Tissue-resident memory T cells can be found within certain locations without recirculating; these cells are typically the first line of defense against pathogens and foreign bodies, especially in locations such as the digestive tract, female reproductive system, lungs, skin, and the brain. The response of these cells is usually faster and more effective than any other memory cell that would travel to the location.
Regulatory T lymphocytes include a subset of lymphocytes involved in maintaining homeostasis of the immune system, modulating the inflammatory response to antigens, and preventing autoimmune reactions and chronic infections. T regulatory cells can also be involved in immunosuppression in organ and tissue grafting and the immune response in cancer growth.
T cells with stem cell-like properties have the potential for regeneration; they are usually found in small amounts and are similar to naïve T cells. These lymphocytes can be quick to respond to viral antigens as well as antigens produced during cancer growth.
B memory cells are also useful to the immune system, with these lymphocytes being involved in the secondary innate humoral response, while memory NK cells are crucial for the workings of the innate immune response, which help fight against viruses and tumorigenesis.
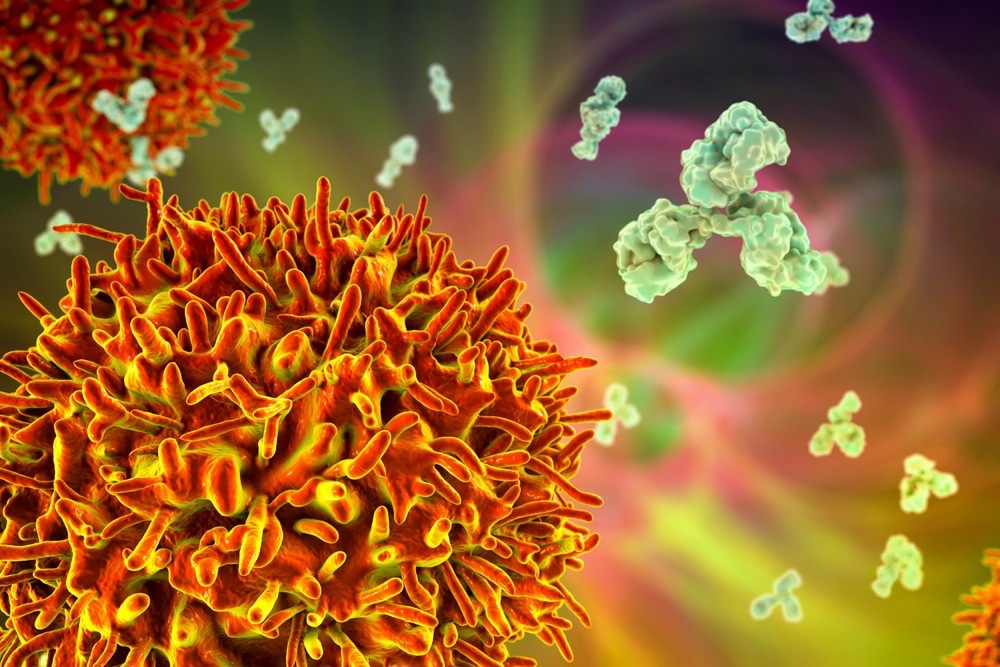
Image Credit: Kateryna Kon/Shutterstock.com
Applications of Immunological Memory and Future Outlook
Immunological memory can provide long-term protection after an infection or vaccination; this is one of the reasons that vaccinations are held in high regard in the scientific community for promoting public health. The development of vaccines and as well as their propagation among children has led to long-term protection against viruses such as measles.
This is also true of other infections and acute infectious diseases that may have resulted in a potentially severe illness before vaccination was widespread. Naturally, the immune system can recognize a foreign antigen in the body, which causes the innate and then adaptive immune response to be activated.
Without the memory immune response, the ability of the body to protect itself from pathogens would be less effective, especially with secondary occurrences of contact with the same antigens.
The development of vaccines has been revolutionary for medicine and the prevention of infectious diseases; however, the widespread of vaccines within less economically developed countries is still challenging. The strength to fight disease is a global issue, and to eradicate viruses and infectious diseases worldwide, further research into accessible medicine is required.
Sources:
- Janeway CA Jr, Travers P, Walport M, et al. Immunobiology: The Immune System in Health and Disease. 5th edition. New York: Garland Science; 2001. Immunological memory. Available from: https://www.ncbi.nlm.nih.gov/books/NBK27158/
- Ratajczak W, Niedźwiedzka-Rystwej P, Tokarz-Deptuła B, Deptuła W. Immunological memory cells. Central European Journal of Immunology. 2018;43(2):194-203. doi:10.5114/ceji.2018.77390
Further Reading
Last Updated: Aug 23, 2022