Mutations that occur in white blood cells can play a major role in abnormal immune profile following hematopoietic stem cell transplantation.
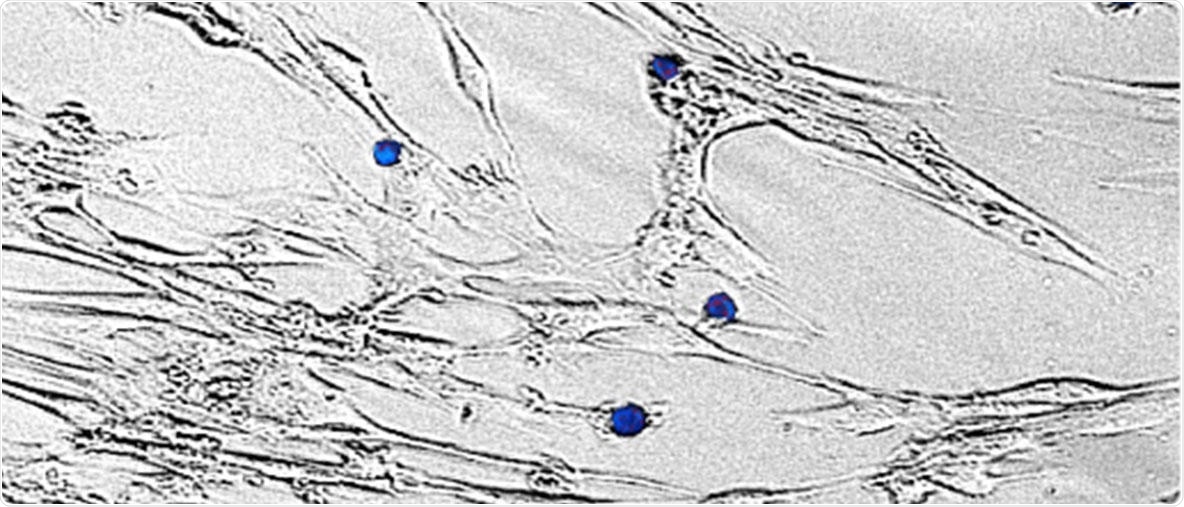
Patient’s CD4+ T cells carrying mTOR mutation attack patient’s own fibroblasts. Image Credit: Daehong Kim.
Graft-versus-host disease, or GvHD for short, is known to be a potentially life-threatening medical disorder that often occurs following allogeneic hematopoietic stem cell transplantation, the only therapeutic treatment available for different types of leukemias.
In GvHD, white blood cells from transplant donors detect recipient cells as non-self and subsequently attack the recipient tissues.
A better understanding of how these donor white blood cells continue to be active against recipient cells can lead to the development of new treatment methods in GvHD.
Headed by Professor Satu Mustjoki at the University of Helsinki, a new research project looked at the role of T cell mutations in GvHD. Cancer cells often contain the somatic or so-called acquired mutations during a lifetime, but not much is known about their existence as well as their importance in other cells, like cells in the defense system of the body.
The study, published in the Nature Communications journal, initially detected an index chronic GvHD patient who had an activating somatic mutation in a gene known as mTOR, which controls the growth and survival of cells.
The study’s authors subsequently screened an international group of 54 healthy blood donors and 135 GvHD patients. With the help of next-generation sequencing, the researchers discovered that 2.2% of chronic GvHD patients harbored a mutation in mTOR, while none of the healthy blood donors reflected this mTOR mutation.
What makes our finding particularly significant is that the mutation now found was recurrent, meaning that the same mutation was found in several patients with chronic GvHD. Our previous studies in rheumatoid arthritis had shown that acquired mutations could be found in T cells, but in these studies, the mutations had been isolated and the same mutations had not been found in more than one patient.”
Satu Mustjoki, Project Lead and Professor, University of Helsinki
Individualized treatments for patients
When the researchers used single-cell RNA sequencing and T cell receptor sequencing on samples obtained from the index patient, they observed that in spite of the immunosuppressive treatment, the mTOR mutated CD4+ T cell clone had expanded over the duration of GvHD, implying that the mutation had played a role in the disease pathogenesis.
The researchers also discovered that the mutation was situated in the so-called cytotoxic T cells, which were able to destroy the body’s own cells. The scientists also studied the mTOR mutation comprehensively by introducing it into a human cell line. Cell proliferation and cell survival were promoted by the activating mTOR mutation.
To identify promising targeted therapies, the scientists carried out a high-throughput drug screen with 527 drugs. The CD4+ T cells of the index patients were susceptible to a certain group of drugs known as HSP90 inhibitors, implying that these drugs could be used for treating GvHD in the days to come.
Our study helps to understand the mechanisms of activation of the immune system in GvHD. Although several different drug combinations have been tried in the treatment of GvHD, using our results, it is possible to find individualized treatments for patients.”
Daehong Kim, Doctoral Candidate, University of Helsinki
Additional studies using larger cohorts of GvHD are required to figure out whether the clonal mutations in T cells alter the clinical outcome, drug responses, and GvHD severity.
Source:
Journal reference:
Kim, D., et al. (2020) Somatic mTOR mutation in clonally expanded T lymphocytes associated with chronic graft versus host disease. Nature Communications. doi.org/10.1038/s41467-020-16115-w.