The concept that cancer development is “monitored and prevented” by the immune system—known as “cancer immune vigilance”—was first suggested at the beginning of the previous century.
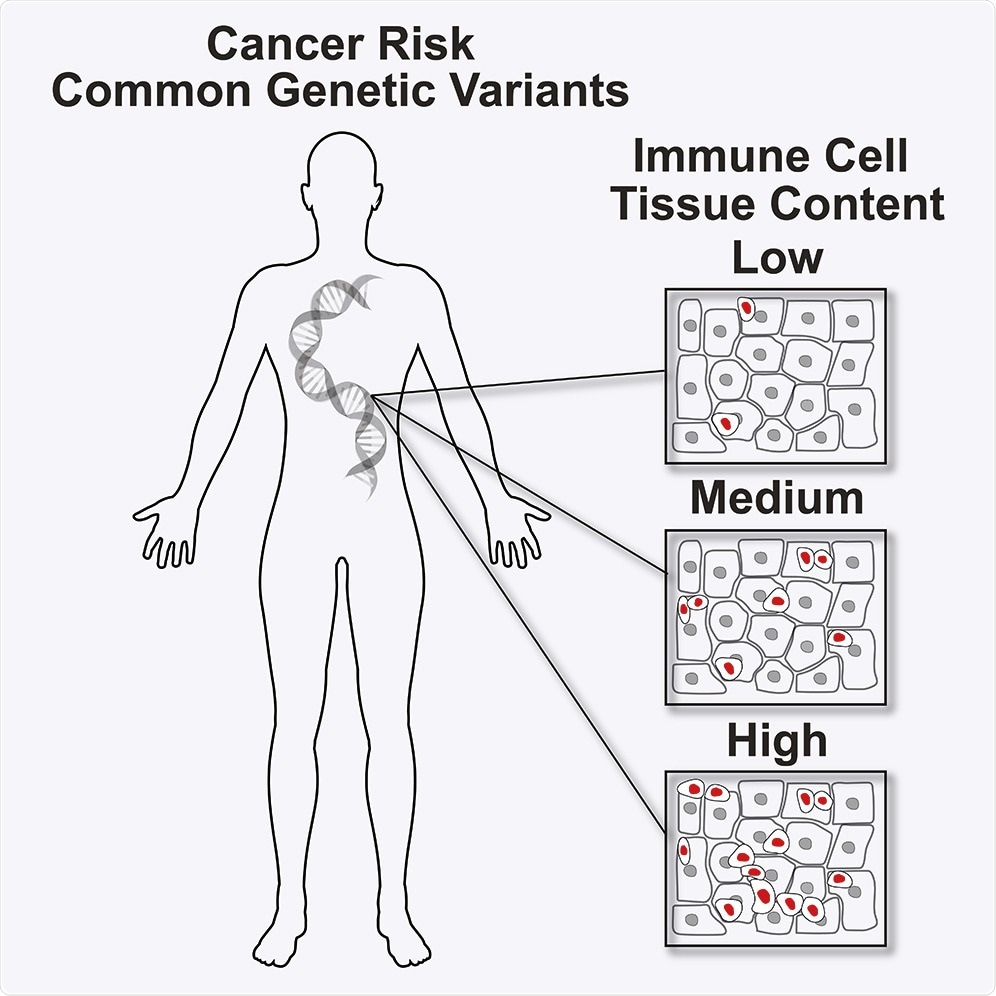
Image Credit: iScience.
Since that time, epidemiological studies have demonstrated that the inhibition of the immune system boosts the risk of cancer, although the molecular basis of this process is yet to be fully understood.
Now, research carried out by an international team, headed by the ProCURE program of the Catalan Institute of Oncology (ICO) and the OncoBell program of the Bellvitge Biomedical Research Institute (IDIBELL), has discovered the genetic variants that predispose individuals to cancer and also denote a modification of the immune system.
The researchers achieved this by examining 17 types of cancer and successfully detected up to 57 genetic variants in 13 types of cancer. These genetic variants predispose individuals to develop cancer and affect their bodies’ defenses.
Published in the iScience journal of the Cell Press editorial, the study represents a major breakthrough in providing a better understanding of the biological bases that trigger cancer and paves the way for upcoming risk analysis. It also enables people to think of novel approaches to prevent this disease.
The results suggest that the risk of developing cancer can be explained, in part, by alterations in the number of immune cells. If we know the effect that these genetic variants have on the immune system, we can design new prevention strategies for patients with a high risk of developing cancer through the modulation of specific functions of the immune system cells.”
Miquel Pujana, Project Leader and Researcher, ProCURE Program, Catalan Institute of Oncology
Pujana also leads the OncoBell program at IDIBELL-Bellvitge Biomedical Research Institute.
One major link identified in this research is the association between the modified function of the SH2B3 gene—a lymphocyte protein—and the chance of developing breast cancer, particularly in women who face an increased risk of getting this kind of cancer, because of mutations that occur in the BRCA1 and BRCA2 genes.
Histochemical studies have confirmed this fact because the modification of the SH2B3 gene is associated with a lower infiltration of immune cells in the tumor tissue—an underlying point to exercise its function.
However, in the presence of this genetic variant, only fewer lymphocytes are present in the peripheral blood, and it is associated with a cancer diagnosis at younger ages.
These indications lead us to think that the correct function of the SH2B3 gene is decisive for the protection of cancer in women carrying BRCA1/2 mutations and, when it is affected, the pharmacological induction of the SH2B3 gene could reduce the risk of cancer.”
Miquel Pujana, Project Leader and Researcher, ProCURE Program, Catalan Institute of Oncology
The immune system in the development of cancer
The immune system, which detects foreign microbes as “not themselves” and triggers a response to kill these disease-causing agents, plays an analogous role in safeguarding the body against malignancies.
Impaired DNA from cancer cells ultimately triggers the synthesis of abnormal proteins called tumor antigens. Such abnormal tumor proteins label the cancer cells as “not themselves.”
While the immune system could identify and destroy cancer cells, these cancer cells have mechanisms that enable them to evade the immune reactions that often inhibit the development of malignant tumors. When the surveillance function is lost by the immune system, tumor cells can develop into a tumor.
Source:
Journal reference:
Palomero, L., et al. (2020) Immune Cell Associations with Cancer Risk. iScience. doi.org/10.1016/j.isci.2020.101296.