AZoLifeSciences speaks to Dr. Tim Blower about his research into tuberculosis, and how the discovery of a new toxin could lead to new anti-TB drugs.
What provoked your research into tuberculosis?
My undergraduate studies sparked an interest in the mechanisms used by bacteria to successfully cause an infection and resist antibiotics. During my postdoctoral Fellowship, with Prof. James Berger at Johns Hopkins University, we developed a project to look at how the tuberculosis bacteria respond to a range of fluoroquinolone antibiotics.
We were able to show that small changes in the antibiotic target drastically limited the impact of the drugs, but by re-designing the antibiotic, we could get around antibiotic-resistance. I have been working on tuberculosis since.
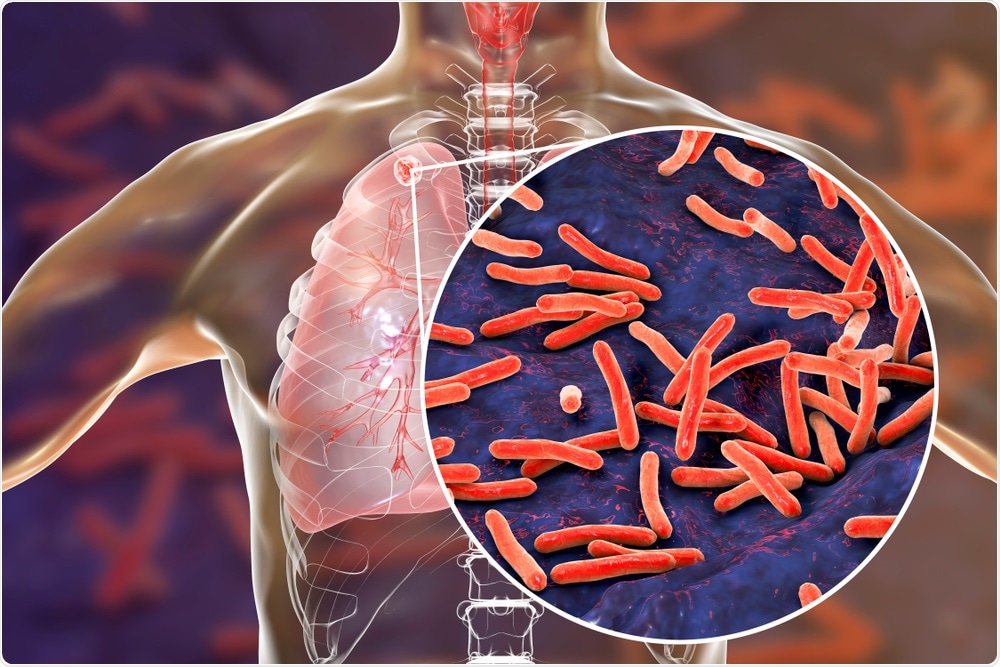
Image Credit: Kateryna Kon/Shutterstock.com
What is tuberculosis and how is it spread?
Tuberculosis is an infection caused by the bacterium Mycobacterium tuberculosis. As of 2018, tuberculosis became the biggest cause of death through infectious disease, on the planet.
An estimated quarter of the world’s population has a latent (dormant) infection in the lungs, with around 10 million people developing active cases annually, leading to 1.5 million deaths each year.
The burden is mostly in sub-Saharan Africa, India, China, and South-East Asia, though there are cases in Europe and the Americas. The infection causes a chronic cough, damage to lung tissue, and weight loss. It also has the potential to spread to other areas of the body. This is an old foe – there is evidence of tuberculosis infections within Egyptian mummies.
Whilst the problem is huge, the good news is that the number of cases is dropping, and the WHO produce a fantastic annual report tracking these efforts. Of course, more work is needed.
Why is the number of antibiotic-resistant tuberculosis infections increasing?
This is a complicated question, which touches on the biochemistry of how the drugs work, and societal pressures. There are two key antibiotics used to treat tuberculosis – rifampicin, and isoniazid. Patients are required to take these drugs for around 6 months.
As this is such a long course of antibiotics, a person might find it hard to access the drugs for the duration or may not be strict about taking them regularly and for the full time. As a result, the antibiotic concentrations drop within the patient, producing the perfect conditions to select for bacteria that have developed resistance.
Multi-Drug Resistant (MDR) tuberculosis bacteria are becoming more widespread and are resistant to both these antibiotics. Further treatment options are available, but extensively drug-resistant and even total drug-resistant bacteria have been identified, which cannot be treated.
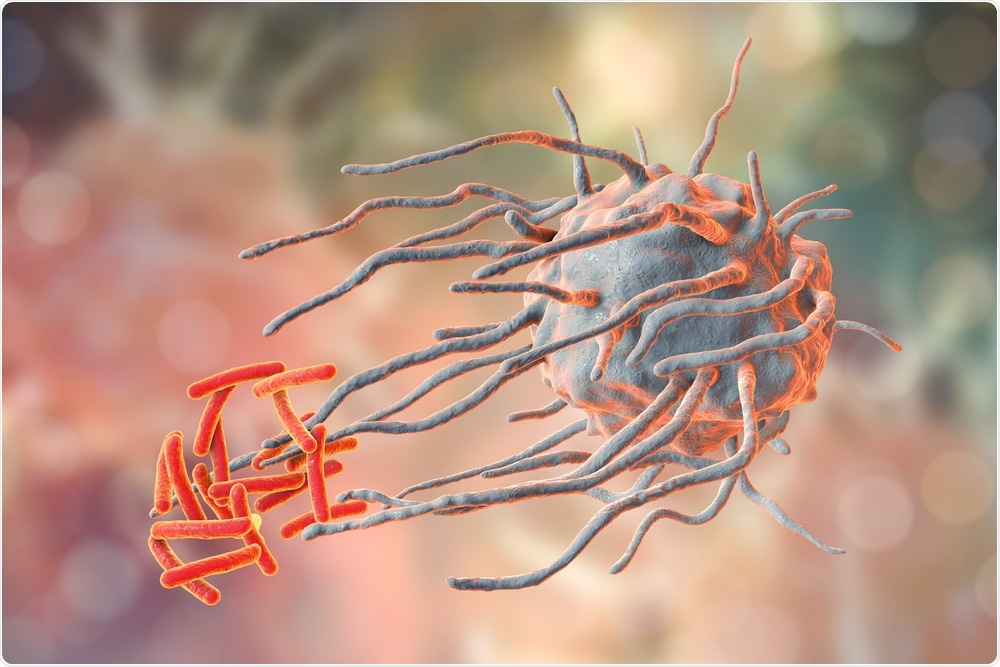
Image Credit: Kateryna Kon/Shutterstock.com
What role do toxins and their counterparts play in tuberculosis infections?
This is a hotly debated topic! Mycobacterium tuberculosis has the largest collection of these toxins and partner antitoxins, of any known bacterial species. There are over eighty of them within M. tuberculosis. We know that the toxins are activated under conditions occurring during infections, such as when the bacteria are engulfed by macrophages of the host’s immune system, or in response to nutrient stresses or antibiotics.
One theory is that the toxins are activated in response to these stresses, which allow the bacteria to go dormant (consider them “undercover”) and survive active killing by the immune system and antibiotics. Over time, the antitoxin will then negate the action of the toxin, allowing the cells to resuscitate and continue the infection. It is an enticing model that is being investigated further by many research labs.
How did you discover the toxin MenT and what is this toxins role in tuberculosis?
The co-lead author on this new work, Dr. Pierre Genevaux (CNRS, Toulouse University, France), had cataloged the toxins within M. tuberculosis, and my long-standing collaborator, Prof. Peter Fineran (University of Otago, New Zealand) had worked on a related system.
We were able to form an international collaboration to look more closely at the MenT family. We now know that MenT, when activated, rapidly reduces the growth of M. tuberculosis. We solved the structure of two related MenT protein toxins (using X-ray crystallography), and we identified how MenT works.
The mechanism has not been described before; MenT will modify tRNAs, by adding additional nucleotides to the acceptor stem. This blocks recognition and charging with amino acids, so there is no pre-cursor charged tRNAs for translation.
As a result, the cell cannot synthesize new protein and will stop growing. The next step is to better understand when this mechanism comes into play during infection.
How could this toxin discovery potentially lead to the treatment of tuberculosis?
The key finding of this work is a new method of killing tuberculosis. Converting this into treatment would of course be a long process. We can learn from the activity of MenT, and now devise new ways to modify and block tRNAs.
It is also possible to imagine several other approaches, wherein you could deliberately activate MenT to force active cells to stop growing, or conversely, block MenT so that cells cannot go dormant. This would then help the immune system or antibiotics to clear the infection.
What further research needs to be carried out before this treatment could be used?
It would be necessary to demonstrate control of MenT toxins. Once we can switch them on and off, on-demand, within M. tuberculosis, we might be able to control the growth of the bacteria.
However, this is a very large task, involving the identification of suitable molecules to bind MenT that are non-toxic to humans.
What are the next steps in your research investigating tuberculosis?
Tuberculosis has been around for thousands of years, it is a successful and complex pathogen. There is lots more to understand about not only the MenT toxins but many of those other toxin-antitoxin systems.
Since these toxins have evolved to have exquisite control over bacterial growth, by exploring the biochemistry and activity of these toxin families, we can learn from nature, taking tried-and-tested concepts into drug development.
Where can readers find more information?
Dr. Tim Blower staff profile
Department of Biosciences, Durham University
Blower Lab website
The Academy of Medical Sciences
About Dr. Tim Blower
Dr. Tim Blower did his undergraduate degrees and Ph.D. at Cambridge University, supervised by Prof George Salmond, winning the Sir Howard Dalton Young Microbiologist of the Year Award in 2009 (Microbiology Society) and the Nat L. Sternberg Thesis Prize in 2011 (Cold Spring Harbor Laboratories, Phage Meeting).
He then obtained an EMBO Long-Term Fellowship to join Prof James Berger's lab at the University of California-Berkeley before moving across to Johns Hopkins University School of Medicine.
Arriving at Durham University in 2015, Tim won a Springboard Award in 2017 (Academy of Medical Sciences) and a Lister Institute Prize Fellowship in 2019 (Lister Institute of Preventive Medicine). He was made an Associate Professor in 2019.