AZoLifeSciences speaks to Dr. James Whittle and Professor Geoff Lindeman about their latest research in enhancing breast cancer therapy through killing 'sleeper cells'.
Why did you choose to research breast cancer?
Breast cancer is the most commonly diagnosed cancer in Australia, and the number of people diagnosed each year is increasing. Despite considerable progress, new strategies are required to address treatment resistance.
As a medical oncologist, I have gained a detailed understanding of some key challenges facing women with breast cancer. These clinical insights have driven my passion for pursuing research that could improve health outcomes for patients.
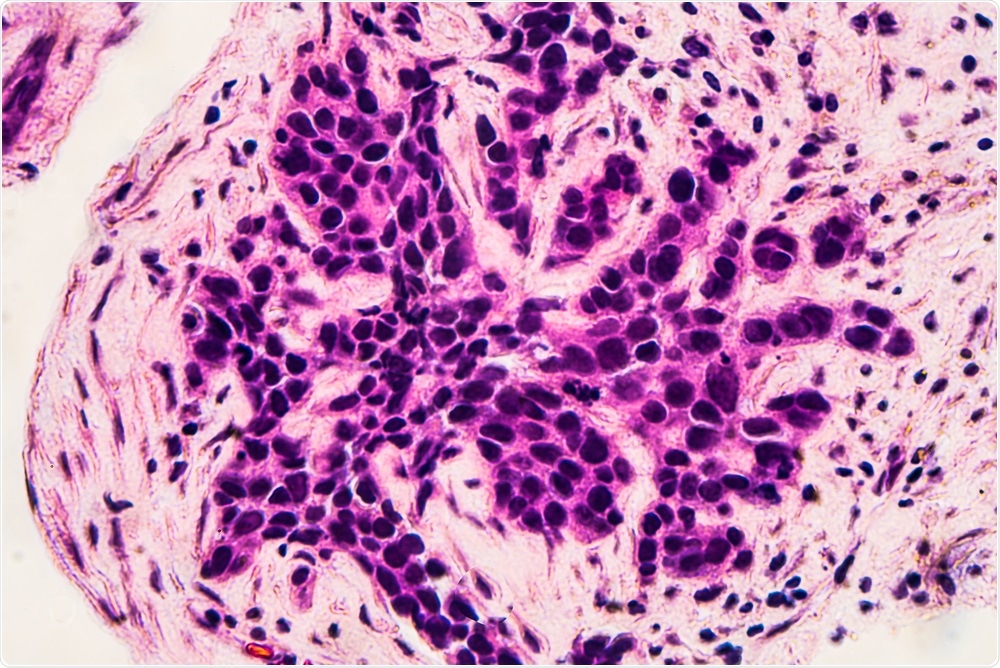
Image Credit: David A Litman/Shutterstock.com
What is estrogen-receptor-positive breast cancer?
Estrogen receptor-positive breast cancer is the most common form of breast cancer and the cancer cells grow in response to the hormone estrogen. This makes cells vulnerable to hormone therapy which stops the estrogen signals which tell a cancer cell to grow.
What are the current therapies used to treat this type of breast cancer?
About 1 in 8 women will be diagnosed with breast cancer in their lifetime and more than two-thirds of these are estrogen receptor-positive. Fortunately, with early detection and modern treatments, most of these women will be cured.
However, there is a proportion of patients whose cancer returns or relapses and spreads to other parts of the body. When this happens therapy may slow the growth of tumors and help women live longer, however relapse is almost inevitable.
Standard treatment for patients whose cancer has relapsed now includes a hormone blocker with a second drug called a CDK4/6 inhibitor.
Why do these current therapies have a high risk of cancer relapse?
The standard of care treatment stops cells from multiplying but there is a lot of room for improvement. The combination works well at slowing growth, however, does not effectively kill cancer cells.
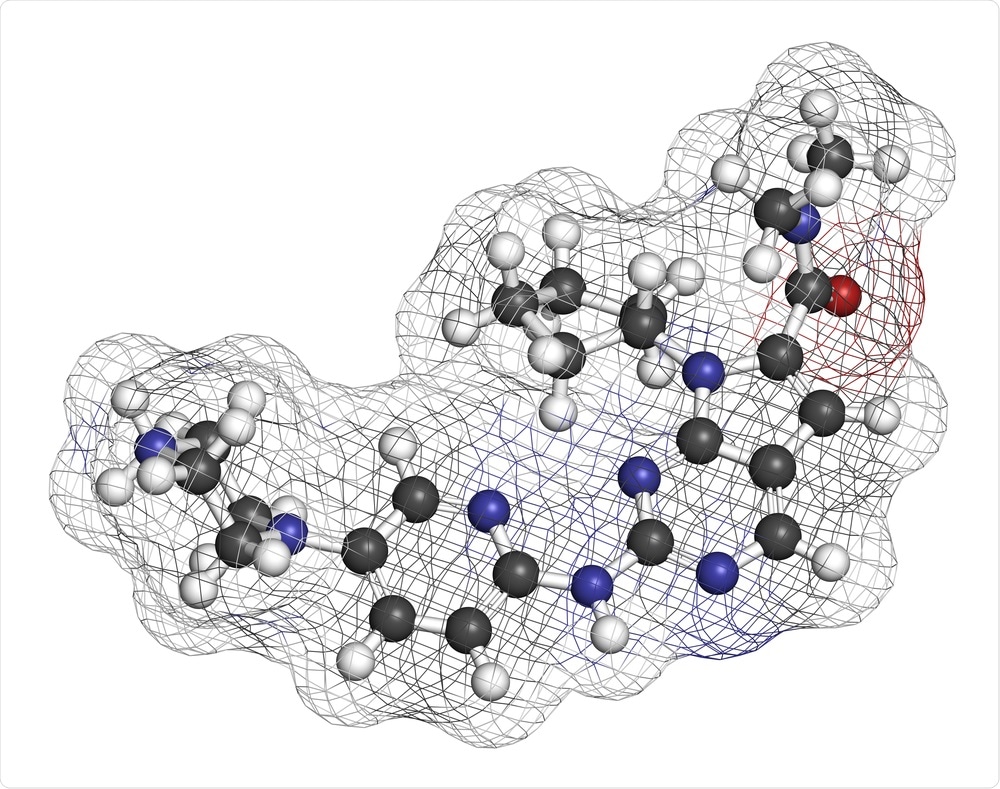
Image Credit: StudioMolekuul/Shutterstock.com
How are cancer cells put to sleep by CDK4/6 inhibitor drugs?
Cancer cells respond to cancer therapy in different ways. These can include slowing cell growth, cell death (also known as apoptosis) and a sleeping state referred to as senescence. Senescence is a state of irreversible growth arrest.
While this can lead to beneficial effects in responding to cancer, when senescent cells accumulate in the body it can attract immune cells leading to inflammation and ‘re-awakening’ of the cancer cells, resulting in relapse. This understanding has prompted many researchers to uncover ways of selectively killing senescent cells.
How could we use venetoclax to kill these sleeping breast cancer cells?
Senescent or “sleeping” cancer cells are relatively resistant to cell death as they often express high-levels of tumor survival (anti-apoptotic) proteins, including BCL2 and BCLXL. It was therefore theorized that these cells might respond to venetoclax which is a potent inhibitor of BCL2.
Can you describe how you carried out your research that led to this discovery?
This research used several laboratory models and focussed on the use of human patient samples and how they respond to treatment.
.jpg)
Image Credit: CI Photos/Shutterstock.com
What did you discover?
Using samples that have been donated from patients with breast cancer adding the anti-cancer drug venetoclax to the gold standard treatment led to a more pronounced and prolonged response to treatment. This is important, given that the current standard treatments are effective in slowing cancer growth but do not kill the cancer cells.
As part of the research, there were several exciting new findings.
- First, the standard treatment can put the cancer cells in a suspended or sleeping state but does not kill them effectively. Adding venetoclax can kill these sleeping cancer cells.
- The combination with venetoclax also enhanced the ability of the immune system to target cancer cells making them responsive to immunotherapy.
Do you believe that this research can help to improve breast cancer therapy?
We are hopeful that this research may improve outcomes for patients with breast cancer, however, it remains to be tested in patients.
To explore this further, we have commenced an early phase clinical trial to test the safety and effectiveness of combination therapy that includes venetoclax.
What are the next steps in your research?
The laboratory research is now being tested in Phase 1 clinical trial PALVEN, being conducted in Melbourne. The first step of a Phase 1 trial is to test whether triple therapy is safe for patients and to identify a suitable dose of drugs.
If the results are promising, the next step would be to consider a larger randomized study to compare the triple combination against the standard of care treatment.
Where can readers find more information?
Please provide links to any materials that may be relevant to our audience.
- For more information about breast cancer
- The paper can be accessed
- For more information about the Visvader / Lindeman laboratory please visit
- For more information about the PALVEN clinical trial please visit
- If patients are interested in the clinical trial we recommend they talk to their oncologists to see if this treatment might be appropriate for them. For referrals
About Dr. James Whittle
Dr. Whittle is an early career clinician-scientist subspecialising in breast cancer and Neuro-Oncology at the Peter MacCallum Cancer Centre. He is currently a postdoctoral research fellow at the Walter and Eliza Hall Institute of Medical Research where his Ph.D. and ongoing research in the Visvader/Lindeman laboratory has focussed on understanding the molecular mechanisms that are responsible for resistance to cell death in breast cancer. 
This work is providing the foundation for testing novel compounds in early phase clinical trials, together with industry collaboration.
Also, he has explored how the accumulation of genetic hits to a key cell of origin could influence the resulting breast cancer subtype. It is anticipated that these insights will substantially advance the understanding of the process of tumor development and lead the way to novel strategies for cancer therapy.
About Professor Geoff Lindeman
Professor Geoff Lindeman is a clinician-scientist who has spent more than 20 years advancing research aimed at delivering better treatments for breast cancer.
Together with Professor Jane Visvader, he co-leads the Cancer Biology and Stem Cells Division at the Walter and Eliza Hall Institute where they have made significant discoveries about how normal and cancerous cells develop in the breast that include;
- Identifying breast stem cells, which give rise to normal tissue.
- Identifying the breast cells that are predisposed to becoming cancerous in women with BRCA1 mutations. The discovery of RANK-positive progenitors as a target for breast cancer prevention in BRCA1 mutation carriers is now being studied in an international phase 3 breast cancer prevention trial, BRCAP.
- Demonstrating the use of patient-derived xenograft (PDX) and organoid models to test novel anticancer agents. This includes pre-clinical studies using BH3 mimetics (which target survival pathways in tumor cells) and has led to early phase clinical trials of the BCL2 inhibitor venetoclax.