Researchers, who performed an elaborate search of genetic variation databases, did not find any major differences across populations and ethnic groups in seven genes linked to the viral entry of SARS-CoV-2.
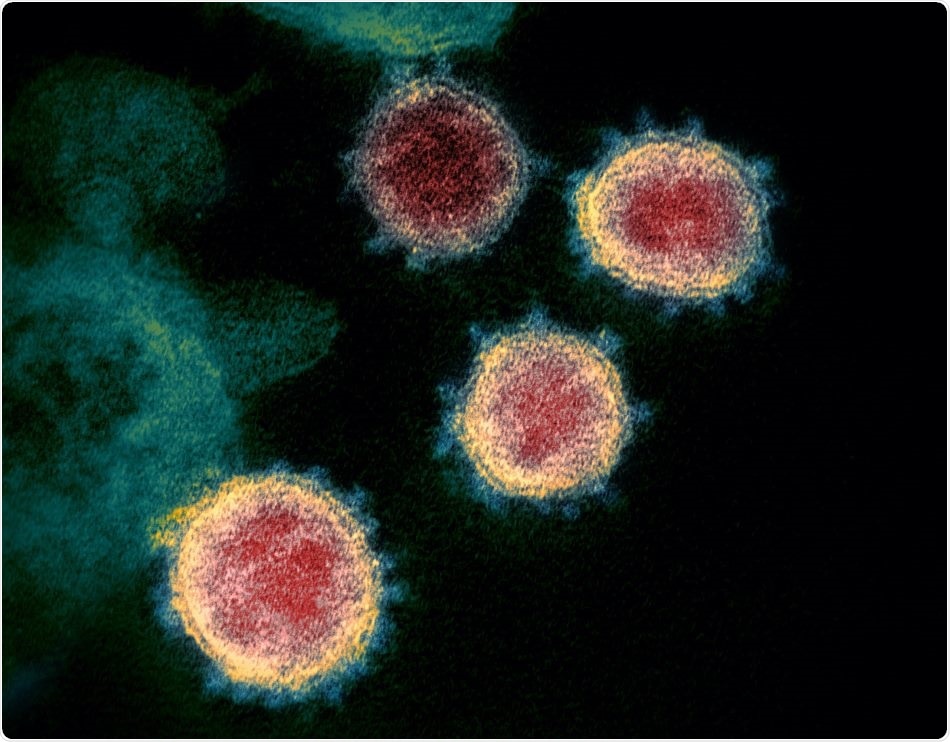
A false-color transmission electron microscope image of SARS-CoV-2. Image Credit: NIAID-RML/Flickr.
Ethnic minorities in the United Kingdom and African Americans and Latinos in the United States are disproportionately impacted by COVID-19. These populations can possibly develop severe symptoms and also exhibit considerably higher mortality when compared to other ethnic and regional groups.
To find out whether this disparity could be caused by genetic changes, a group of three researchers—including Assistant Professor Ji-Won Lee from Hokkaido University’s Graduate School of Dental Medicine—surveyed freely available databases of genomic variants, such as the Korean Reference Genome Database gnomAD; a Japanese genetic variation database TogoVar; and the 1000 Genomes Project.
The researchers analyzed variants across numerous ethnic and regional groups in seven genes that are known to play crucial roles in viral access into host cells and in the detection of viral RNA in host cells.
SARS-CoV-2 contains spiked protein (S protein) on its envelope, which encapsulates the virus. Just before the virus can penetrate the host cells, the S protein has to attach to the ACE2 receptor on the surface of the cell.
Later, it is broken into two parts by the enzymes cathepsin B and L and TMPRSS2. Once the virus penetrates the cells, the viral RNA attaches to the TLR3, TLR7, and TLR8 proteins and subsequently triggers an innate immune response.
According to the study results, these seven proteins had genetic variants, with ACE2 having the largest number of variants. However, only a few of these variations modify the functions of these proteins. As the entire variation frequency was very low (less than 0.01%), the researchers determined that there is no major variations across populations or ethnic groups in relation to the functions of the seven proteins involved in infection.
The findings made by the team indicate that variations in mortality and morbidity are not the outcome of genetic variations in genes for viral entry through populations but rather pre-existing medical conditions, environmental factors, individual medical histories, and healthcare disparities could have played a major role in affecting the mortality and morbidity of COVID-19.
But due to the reduced size of the population databases employed in this study, more studies using more different human genome databases are needed. Other studies have also demonstrated that genetic factors may contribute to serious COVID-19 cases.
Source:
Journal reference:
Lee, I-H., et al. (2020) A survey of genetic variants in SARS-CoV-2 interacting domains of ACE2, TMPRSS2 and TLR3/7/8 across populations. Infection, Genetics and Evolution. doi.org/10.1016/j.meegid.2020.104507.