Adoptive transfer of T-cells can extend survival and, at times, treat patients with advanced solid tumors. Although this method sounds promising, it may take months to create the required T-cells to aid these patients. Such a slow rate renders this treatment unfeasible for a majority of the patients who require immediate treatment.
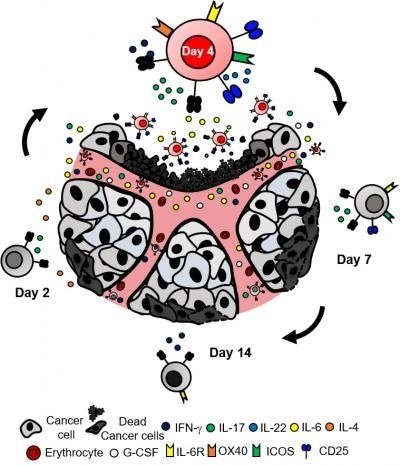
A faster approach for T-cell therapy against cancer. Knochelmann and colleagues show a subset of CD4 T-cells, Th17 cells, can effectively kill tumor cells when they are grown in cell culture for only four days. Th17 cells grown for shorter or longer periods of time cannot successfully eradicate the tumor. Additionally, the cytokine IL-6 is produced by the day-four Th17 cells, which supports the tumor-eradicating functions of the Th17 cells. Image Credit: Medical University of South Carolina Hollings Cancer Center.
In the September issue of Cancer Research, Hannah Knochelmann, a researcher in Chrystal Paulos’ laboratory and a student in the Medical Scientist Training Program at the Medical University of South Carolina (MUSC), joined researchers from three different NCI-designated cancer centers—Medical University of South Carolina Hollings Cancer Center, Emory Winship, and the James at The Ohio State University—to report a novel method for producing T-cells faster for patients in the upcoming days.
The human immune system has two main types of T-cells, known as CD4 and CD8. The research group reduced the time required to produce T-cells from many months to less than a week by employing an exceptionally potent CD4 T-cell subset, known as Th17 cells.
In fact, very few Th17 cells were needed to eradicate multiple different types of tumors effectively. This new milestone could widen inclusion criteria to promote access to T-cell therapy for more patients with metastatic disease.”
Hannah Knochelmann, Student, Medical Scientist Training Program, Medical University of South Carolina
Adoptive T-cell transfer treatment, in which therapeutic T-cells are transferred into a patient, is utilized in only a few institutions worldwide. This renders a potent treatment inaccessible for the general public. Such procedures frequently use an unlimited number of CD8 T-cells, which have cytotoxic characteristics that enable them to destroy tumor cells.
But it takes weeks of growth in cell culture to grow CD8 T-cells that are sufficient to be employed in a single therapy.
What is most remarkable about this finding is that we can build on this platform to bring T-cells to patients all over the world.”
Chrystal Paulos, Director of Translational Research for Cutaneous Malignancies, Emory University
Paulos is also Knochelmann's mentor.
The best effector Th17 cells are cultured in cell culture for just four days before they are infused into the host. Any shorter or longer time in cell culture decreased the treatment efficacy. Although the group could produce more numbers of Th17 cells across several weeks, more cells were actually less or equally effective when compared to fewer Th17 cells that were extended to only four days. This discovery underscored the prospect that T-cell therapy can be given to patients sooner, a finding that hold instant clinical implications.
Another major drawback of traditional T-cell therapy is that patients can relapse—that means, cancer can return even after apparently successful treatment. Hence, Knochelmann and the group sought to design a treatment that lasts for a long time while figuring out factors that can avoid relapse.
The team discovered that a long-lasting response is provided by day-four Th17 cell therapy. Fascinatingly, IL-6 was a crucial cytokine in driving these T-cells to avoid relapse following treatment. This cytokine undermined the regulatory T-cells—the brakes of the immune system—which empowered the Th17 cells to destroy tumor cells.
Paulos informed that the team wants this information to encourage physicians with a new method of thinking about immunotherapy.
He added, “This treatment has the potential to be very versatile. If the tumor can be targeted, meaning that a unique identifier for the tumor is known, this treatment can be effective. Thus, this therapy can be used to treat patients with either liquid or solid tumors.”
According to Knochelmann, the research environment and key facilities at Medical University of South Carolina were a significant piece for the success of this study..
Many colleagues gave me key advice on this discovery. In fact, this work is a great example of what can be accomplished when different minds come together. It has been inspiring and rewarding to work on improving medicine for the future.”
Hannah Knochelmann, Student, Medical Scientist Training Program, Medical University of South Carolina
The study was financially supported by the National Institutes of Health and the Melanoma Research Foundation, as independent grants were given to both Knochelmann and Paulos. At present, the team is working with medical oncologists and surgeons to develop their discoveries into relevant therapies for patients.
“Our vision is that T-cell products will be generated for patients within a few days, so these therapies can help all patients in need, especially those needing treatment quickly,” Knochelmann concluded.
Source:
Journal reference:
Knochelmann, H. M., et al. (2020) IL6 Fuels Durable Memory for Th17 Cell–Mediated Responses to Tumors. Cancer Research. doi.org/10.1158/0008-5472.CAN-19-3685.