Image Credit: Babraham Institute
The researchers’ study adds to the emerging picture of the immune system response and humans’ interpretation of the immunological traits related to the development of serious and fatal disease after COVID-19. Such an understanding is very important to direct the expansion of effective healthcare and “early-warning” systems to detect and treat individuals at risk of a severe response.
One of the most enigmatic questions about the COVID-19 pandemic around the world is why people show such a varied response.
A few individuals do not display any symptoms, called “silent spreaders,” while some patients affected by COVID-19 infection need intensive care support because they develop an extreme immune response.
While it is known that underlying health conditions and age can raise the risk of severe response, the fundamental reasons for the hyperactive immune response observed in certain persons remain unclear, although this might be due to several factors contributing collectively.
To examine the differences in the immune system that may shed light on the spectrum of responses, researchers from the VIB Centre for Brain and Disease Research and KU Leuven in Belgium and also from the Babraham Institute in the United Kingdom collaborated with CONTAGIOUS consortium members to compare the immune system response to COVID-19 infection in patients displaying mild-moderate or severe effects, utilizing healthy individuals as a control group.
One of our main motivations for undertaking this research was to understand the complexities of the immune system response occurring in COVID-19 and identify what the hallmarks of severe illness are. We believe that the open sharing of data is key to beating this challenge and so established this data set to allow others to probe and analyse the data independently.”
Adrian Liston, Professor and Senior Group Leader, Babraham Institute
In particular, the investigators looked at the presence of T cells—which are essentially immune cells with a varied set of functions relying on their sub-type, with “cytotoxic” T cells that can directly destroy virus-infected cells, while other types of “helper” T cells control the action of other immune cells.
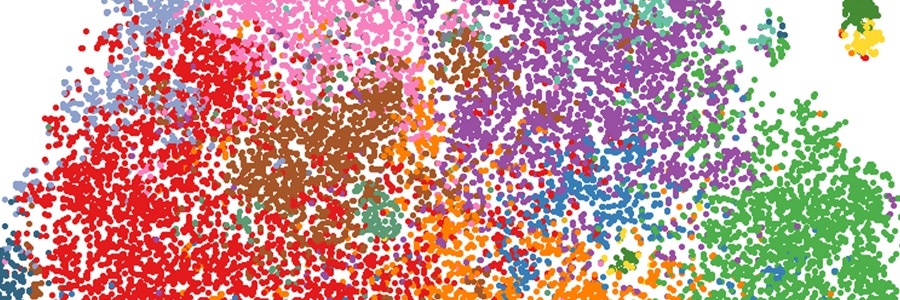
Flow cytometry was used by the researchers to isolate the target cells from the participants’ blood. This was done based on cell activation markers, T cell identification markers, and cytokine cell signaling molecules.
Unexpectedly, the T cell response in the blood of COVID-19- infected patients, categorized as severe, displayed minimal differences in comparison to healthy individuals. This response is contrary to what would often be observed following a viral infection, for example, the flu.
But the team found that the number of T cells had increased, creating a suppressor of cell inflammation, known as interleukin 10 (IL-10). The production of IL-10 is a hallmark of activated regulatory T cells found in tissues like the lungs.
Although rare in healthy persons, the investigators were able to find that the number of T cells has considerably increased in patients with severe COVID-19.
Perhaps, tracking the level of IL-10 may offer a warning about the progression of the disease, but according to the team, larger-scale analyses are needed to validate these findings.
We’ve made progress in identifying the differences between a helpful and a harmful immune response in COVID-19 patients. The way forward requires an expanded study, looking at much larger numbers of patients, and also a longitudinal study, following up patients after illness. This work is already underway, and the data will be available within months,”
Stephanie Humblet-Baron, Professor, KU Leuven in Belgium
“This is part of an unprecedented push to understand the immunology of COVID-19. Our understanding of the immunology of this infection has progressed faster than for any other virus in human history – and it is making a real difference in treatment. Clinical strategies, such as switching to dexamethasone, have arisen from a better understanding of the immune pathology of the virus, and survival rates are increasing because of it,” concluded Professor Liston.
Source:
Journal reference:
Neumann, J., et al. (2020) Increased IL‐10‐producing regulatory T cells are characteristic of severe cases of COVID‐19. Clinical & Translational Immunology. doi.org/10.1002/cti2.1204.