Researchers from the University of Cincinnati (UC) have found new clues about why certain individuals with head and neck cancer are able to respond to immunotherapy, while others fail to do so.
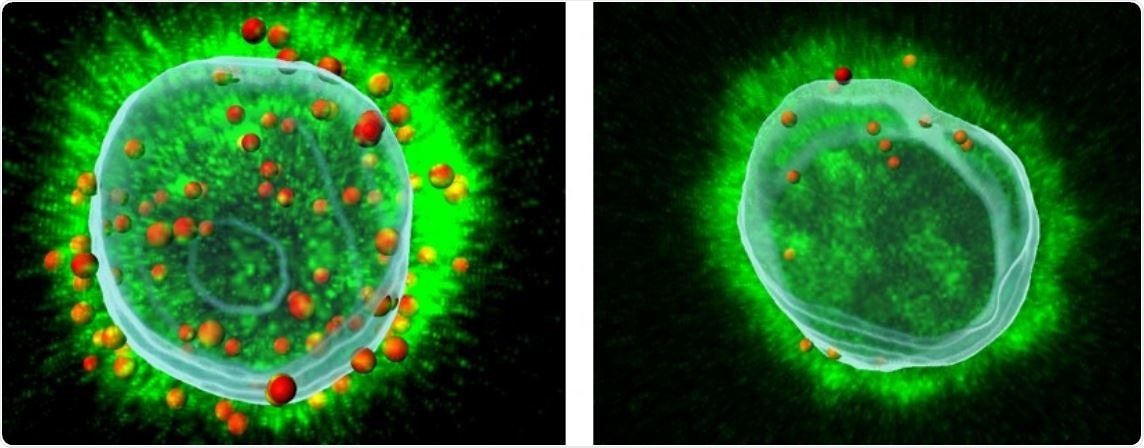
Image of a healthy T cell on the left compared to a cancer T cell on the right. Image Credit: Ameet Chimote.
Published in the Journal for ImmunoTherapy of Cancer, the latest findings demonstrate that this difference in immunotherapy could be due to “channeling” the function and power within a specific kind of immune cell.
Laura Conforti, Ph.D., a professor in the Department of Internal Medicine at the UC College of Medicine and the study’s corresponding author, stated that interpreting these mechanisms could enable the development of combination therapies to treat certain cancer patients more effectively.
Professor Conforti further pointed out that head and neck cancers are the world’s sixth most common cancers and affect around 53,000 Americans per year. Hence, to fight this deadly disease, physicians usually implement immunotherapy, which improves the body’s own immune system in an attempt to detect and destroy tumor cells.
Our immune cells are naturally programmed to distinguish between our body’s ‘normal’ cells and what they see as ‘foreign’ cells and attack only the foreign cells.”
Laura Conforti, PhD, Professor, Department of Internal Medicine, College of Medicine, University of Cincinnati
She added that the immune cells—known as T cells—lead the body’s defense against cancers; however, the effect of that attack can become ineffective if a molecule in tumor cells attaches to an immune checkpoint in the T cells and successfully “turns them off like a light switch.”
Consequently, the T cells cease to attack the tumor cells, which, according to Professor Conforti, is “a major problem,” particularly for head and neck cancers.
Pembrolizumab is a familiar immunotherapy treatment that targets the checkpoint molecule and effectively inhibits the “off switch” of the T cells; however, researchers are looking for ways to find out why this specific approach works in certain individuals and not in others.
Professor Conforti further elaborated that the potential of these T cells to attack and kill tumor cells depends on molecules, known as potassium ion channels. These ion channels are found in T cells and account for a wide range of functions, such as destroying the tumor cells.
Conforti’s group includes the study’s co-lead authors Hannah Newton, Ph.D., a recent doctoral graduate from UC; Vaibhavkumar Gawali, Ph.D., postdoctoral fellow; and Ameet Chimote, Ph.D., a research scientist working in Conforti’s laboratory.
The research team observed that when immunotherapy was given to patients afflicted with head and neck cancer at UC Medical Center, T cells in these individuals demonstrated a high level of activity in these channels, enabling them to reach and destroy the cancer cells more effectively.
The group also observed that once the treatment was given to patients, the ion channels present in the blood-circulating T cells were more active, which means, they are more capable of sustaining their attack against the tumor cells.
We also saw that head and neck cancer patients who were responding to this immunotherapy, meaning their tumors were shrinking, had greater channel activity in their T cells soon after treatment, and the T cells had more ability to enter into the tumors to continue killing cancer cells. However, patients who did not respond lacked this increased activity.”
Laura Conforti, PhD, Professor, Department of Internal Medicine, College of Medicine, University of Cincinnati
Professor Conforti continued, “Immunotherapy is not one-size-fits-all, since some patients respond to immunotherapy, while others don’t, but our research shows that ion channels within T cells of these patients play a crucial role in the response of immunotherapy. Now that we know the benefits of these channels, more research is needed to look at ways we can activate them or create combination therapies to help patients increase their chance of survival.”
According to Newton, a team member, who recently finished her doctorate at UC and currently working at the National Institutes of Health-sponsored Frederick National Laboratory for Cancer Research, working on this research work at UC proved to be quite invaluable.
This research allowed me to collaborate with diverse professional individuals including medical oncologists, clinical coordinators and other researchers and gave me the opportunity to better understand the bench-to-bedside procedure for drug development. Most importantly, it could help clinicians determine more personalized and effective treatment combinations for patients with head and neck cancer.”
Hannah Newton, PhD, Doctoral Graduate, Frederick National Laboratory for Cancer Research
Immunotherapy to fight cancer
Video Credit: University of Cincinnati.
Source:
Journal reference:
Newton, H. S., et al. (2020) D1 blockade enhances K+ channel activity, Ca2+ signaling, and migratory ability in cytotoxic T lymphocytes of patients with head and neck cancer. Journal for ImmunoTherapy of Cancer. doi.org/10.1136/jitc-2020-000844.