A study recently published in the Nature journal has revealed how chemicals in the regions surrounding tumors, called the tumor microenvironment, undermine the immune system and allow cancer to resist attack. These results indicate that an existing medication could improve cancer immunotherapy.
A study led by immunology’s Greg Delgoffe and published in Nature shows how chemicals in the areas surrounding tumors subvert the immune system and enable cancer to evade the attack. These findings suggest that an existing drug could boost cancer immunotherapy. Image Credit: UPMC, created with BioRender.com.
The research was performed by a group of scientists from the UPMC Hillman Cancer Center and the Pittsburgh School of Medicine, headed by Greg Delgoffe, PhD, an Associate Professor of Immunology from the University of Pittsburg.
When the researchers disrupted the impact of the tumor microenvironment on immune cells in mice, they were able to reduce the size of tumors, extend survival, and improve immunity to immunotherapy.
The majority of people don't respond to immunotherapy. The reason is that we don't really understand how the immune system is regulated within this altered tumor microenvironment.”
Greg Delgoffe, PhD, Associate Professor of Immunology, University of Pittsburg
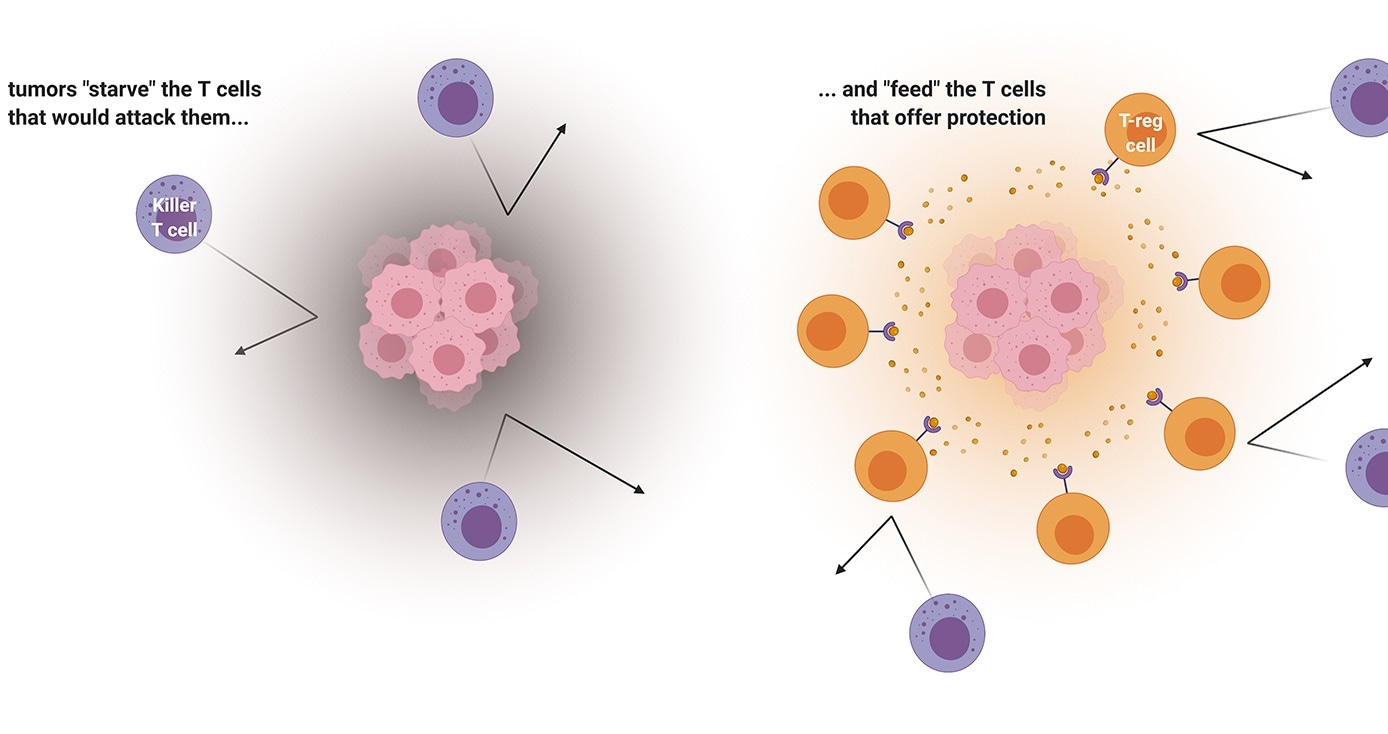
The immune system is composed of several types of cells, and prominent among them are the T cells. One type of cell, known as killer T cells, attacks predators, like bacteria, viruses, and even cancer. Another type of cell, termed regulatory T cells, or T-reg cells for short, counteracts the killer T cells by serving as guardians of cells belonging to the body.
T-reg cells are crucial for the prevention of autoimmune diseases, like multiple sclerosis Crohn's disease, and type I diabetes, in which overactive killer T cells attack the healthy tissues of the body.
To do their jobs, all these different immune cells need to generate energy. Delgoffe’s research team looked at how these different kinds of T cells have different appetites, and the way tumors—which have huge appetites—fight for nutrients with infiltrating immune cells. The team observed that regulatory T cells and killer T cells have extremely different appetites, and this fact is exploited by cancer cells.
Cancer is wise to the whole situation. Cancer cells don't just starve T cells that would kill them but actually feed these regulatory T cells that would protect them.”
Greg Delgoffe, Ph.D., Associate Professor of Immunology, University of Pittsburg
In brief, Delgoffe’s research team observed that tumors ingest all the essential nutrients in their surrounding area that killer T cells would need to fight off. Besides this, tumors also excrete lactic acid, which sustains the regulatory T cells, persuading them to stand guard.
Image Credit: Nathan Devery/Shutterstock.com
Using a protein known as MCT1, T-regs can convert lactic acid into energy, so snuggling up with the tumor is an excellent way for these immune cells to remain fed.
“What better way to recruit a cell than food?” added Delgoffe.
The researchers then used mice with melanoma and observed that silencing the gene that codes for the specific MCT1 protein delayed the growth of tumors and added to this, the mice also lived for a longer time.
We starved the T-regs. When T-reg cells are not being sustained by the tumor, killer T cells can come in and kill the cancer.”
Greg Delgoffe, Ph.D., Associate Professor of Immunology, University of Pittsburg
Most significantly, when Delgoffe’s research team merged immunotherapy with MCT1 inhibition, the anti-cancer effects were stronger than either approach alone.
From the clinical standpoint, the same effect could be achieved by using medications that block the MCT1 protein, one of which is now being tested in patients with advanced lymphoma and it seems to be well-tolerated.
Source:
Journal reference:
Watson, M. J., et al. (2021) Metabolic support of tumor-infiltrating regulatory T cells by lactic acid. Nature. doi.org/10.1038/s41586-020-03045-2.