According to the findings of a recent cell study, the SARS-CoV-2 spike protein can trigger long-term gene expression changes. The results may help understand why certain COVID-19 patients, known as COVID long-haulers, suffer symptoms like dizziness and shortness of breath long after the infection has cleared.
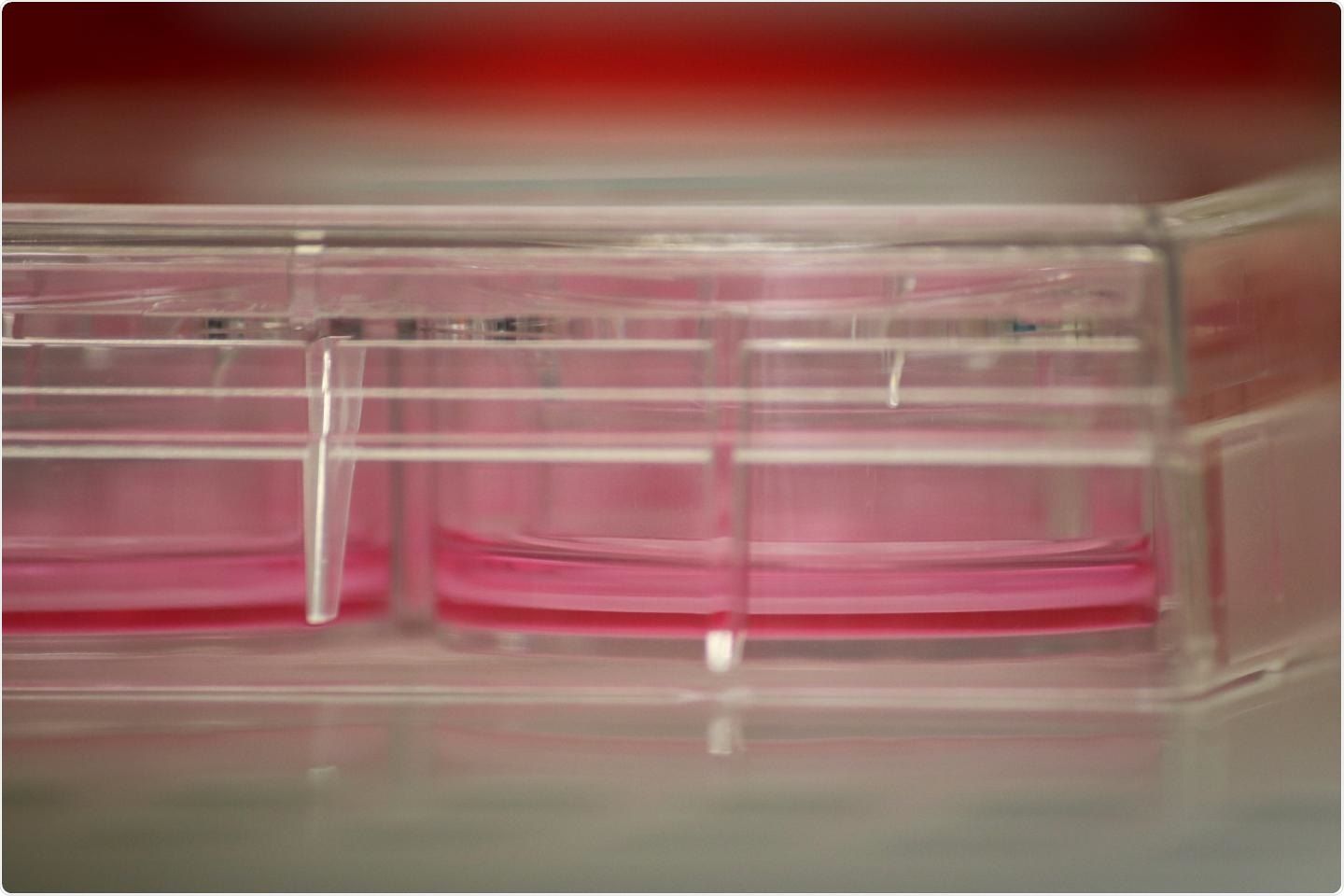
A six-well plate with Transwells inserted. Cells are grown on top of the Transwell, with media to feed them below. Image Credit: Nicholas Evans.
The virus that activates COVID-19, SARS-CoV-2, is wrapped in tiny spike proteins. When the virus causes infection, the spike proteins attach to receptors on the body’s cells, initiating a mechanism that causes the virus to unleash its genetic material into the inner side of the healthy cell.
We found that exposure to the SARS-CoV-2 spike protein alone was enough to change baseline gene expression in airway cells. This suggests that symptoms seen in patients may initially result from the spike protein interacting with the cells directly.”
Nicholas Evans, Master’s Student, Laboratory of Sharilyn Almodovar, PhD, Texas Tech University Health Sciences Center
Evans will discuss the findings at the American Society for Biochemistry and Molecular Biology annual conference, held from April 27th to April 30th, as part of the virtual Journal of Experimental Biology meeting.
The culture of human airway cells necessitates maintaining certain conditions to enable cells to mature into the differentiated cells present in the airway. The research team improved a culturing method called air-liquid interface methodology developed earlier to better mimic the physiological conditions present in the lung airway.
This process involved the exposure of cells to air and then allowing them to develop into airway cells.
The researchers discovered that when cultured human airway cells were exposed to high and low concentrations of purified spike protein, there were variations in gene expression that persisted long after the cells recovered from the exposure. Among the top genes were those associated with the inflammatory response.
Our work helps to elucidate changes occurring in patients on the genetic level, which could eventually provide insight into which treatments would work best for specific patients.”
Nicholas Evans, Master’s Student, Laboratory of Sharilyn Almodovar, PhD, Texas Tech University Health Sciences Center
Moreover, the team made a comparison between their cultured human airway cells with previous experiments in which cells were harvested from patients infected with COVID-19. They could confirm that the optimized cell culture strategy accurately mirrored what happens in patients, making it useful for future translational research.
They want to use the new method to learn more about how long the genetic modifications persist and the possible long-term effects of these changes in long-term COVID-19 situations.