According to a new study, targeting a pathway that is critical for the survival of some cases of acute myeloid leukemia could open up a new therapeutic route for patients.
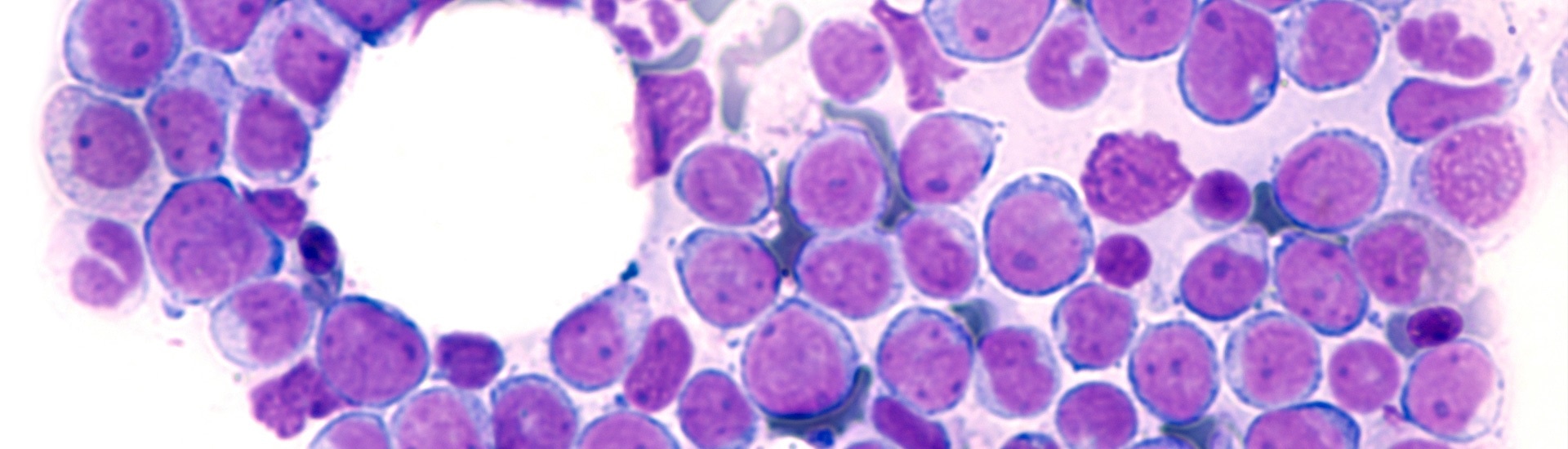
Image Credit: Wellcome Trust Sanger Institute.
A research team from the Wellcome Sanger Institute discovered that a specific genetic mutation associated with a weak prognosis in blood cancer, in human and mice cell lines, is implicated in the disease’s progression when paired with other mutations.
The research, which was published on April 30th, 2021, in Nature Communications sheds more light on how a loss-of-function mutation in the CUX1 gene contributes to the development and survival of acute myeloid leukemia.
The results imply that targeting a pathway required for these cancer cells to develop could give rise to new targeted therapies for certain patients.
Acute myeloid leukemia (AML) is a deadly blood cancer that affects people of all ages and sometimes necessitates months of intensive chemotherapy and lengthy hospitalizations. It normally occurs in bone marrow cells, crowding out healthy cells and resulting in life-threatening bleeding and infections.
For decades, mainstream AML therapies have been stagnant, and less than one in three individuals survive cancer.
Previously, researchers at the Wellcome Sanger Institute USED large-scale DNA sequencing analysis and discovered that loss-of-function mutations in the CUX1 gene on chromosome 7q were present in many forms of cancer, like AML, where it is linked with a weak prognosis. However, the function of this gene in the development of AML is unknown.
The researchers used CRISPR/Cas9 gene-editing technology in this new research to demonstrate that a lack of functional CUX1 contributes to the expansion of some forms of blood stem cells that are defective in a kind of controlled cell death called apoptosis.
They discovered that the loss of CUX1 induces enhanced expression of the CFLAR gene, which encodes a protein that inhibits apoptosis, possibly allowing mutant cancer cells to avoid propagation and cell death.
The research team demonstrated that targeting CFLAR, or apoptosis evasion mechanisms in general, may be a potential therapy for those suffering from this type of AML, which is associated with a poor prognosis. There are currently no clinically accepted drugs that target CFLAR.
By investigating the role of CUX1 further, we now have new insight into how this gene, and the lack of it when mutated, plays a key role in the survival of blood cancer cells. While this mutation doesn’t seem to cause the development of malignant disease on its own, focusing on the pathways involved with CUX1 is a good target for further research.”
Dr Saskia Rudat, Study Co-First Author and Postdoctoral Fellow, Wellcome Sanger Institute
According to Dr Emmanuelle Supper, co-first author and Postdoctoral Fellow at the Wellcome Sanger Institute, “By building on our previous analysis, this research has allowed us to gain crucial information about the development of this disease and would not have been possible without the new and exciting CRISPR/Cas9 and genome sequencing technologies that enable us to investigate genetic weaknesses in cancer.”
“Understanding more about the genetic basis of disease, and how multiple mutations come together to cause blood cancer is vital if we hope to save lives in the future,” added Dr Supper.
Acute myeloid leukemia is a devastating disease, which is currently difficult to treat, especially in cases characterized by genetic lesions such as loss of CUX1 and chromosome 7q deletions. This new study provides evidence that could be used to help develop new targeted treatment for some people living with acute myeloid leukemia, offering hope for this group of patients who unfortunately are more likely to have a poor prognosis.”
Dr Chi Wong, Study Senior Author and Wellcome Clinical Fellow, Wellcome Sanger Institute
Dr Wong is an Honorary Consultant Hematologist at Addenbrooke’s Hospital.
Source:
Journal reference:
Supper, E., et al. (2021) Cut-like homeobox 1 (CUX1) tumor suppressor gene haploinsufficiency induces apoptosis evasion to sustain myeloid leukemia. Nature Communications. doi.org/10.1038/s41467-021-22750-8.