Recent research carried out by the UT Southwestern dermatologists indicates that a familiar inflammatory skin condition might arise due to inadequately regulated sex hormones. The results of the study can provide an unanticipated novel target to combat this condition.
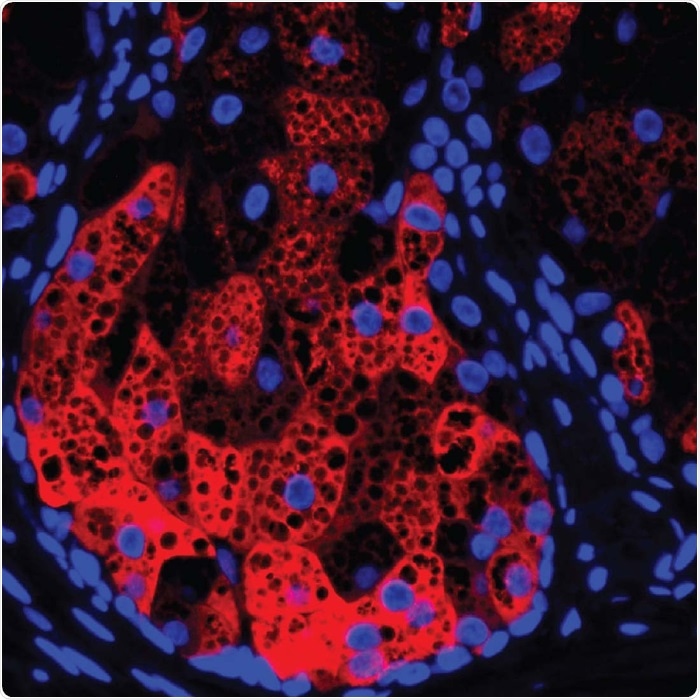
HSD3B1 (red) within a human sebaceous gland, cell nuclei (blue), and lipid droplets (black circular areas). Image Credit: UT Southwestern Medical Center.
The observation was published in the Proceedings of the National Academy of Sciences.
Atopic dermatitis (AD) is a kind of eczema that affects around 13% of children and 10% of adults. The treatment cost for a year is $5.3 billion in the United States.
We often think of eczema as a dry-skin condition and treat mild cases with moisturizers. Here, we’re showing that a gene that’s important for making sex hormones seem to play a role in the skin making its own moisturizers. If we could alter this gene’s activity, we could potentially provide relief to eczema patients by helping the skin make more oils and lipids to moisturize itself.”
Tamia Harris-Tryon MD, PhD, Study Corresponding Author and Assistant Professor, Dermatology and Immunology, UT Southwestern Medical Center
Dr. Harris-Tryon elaborated that earlier studies associated AD with overactivity in genes accountable for the production of two inflammatory immune molecules—interleukins 4 and 13 (IL-4 and IL-13).
A comparatively novel drug named dupilumab—a monoclonal antibody that decreases the amount of the inflammatory molecules—has been exceptionally efficient in numerous patients with mild to severe AD. But the molecular mechanisms behind IL-4 and IL-13 contributing to this form of eczema were unclear.
To explore the question, Dr. Harris-Tryon and her co-workers concentrated on sebocytes-cells that constitute sebaceous glands. The sebaceous glands produce a waxy, oily barrier that coats the skin so that the skin retains its moisture.
Human sebocytes cultured in the Petri dishes were dosed with IL-4 and IL-13, and later, the researchers employed a process named RNA sequencing to obtain a readout on gene activity for the complete genome. They then matched with gene activity in sebocytes that were not treated with these immune molecules.
The researchers identified that a gene named HSD3B1, which produces an enzyme named 3b-hydroxysteroid dehydrogenase 1, was more active (up to 60 times) when exposed to the two interleukins.
According to Dr. Harris-Tryon, the observation was a surprise as the enzyme is widely known for playing a major role in the production of sex hormones like progesterone and testosterone. However, this enzyme was never associated with skin lipid production and atopic dermatitis.
Databases of human gene activity revealed that HSD3B1 is prone to be overactive in patients with eczema. Single research of patients on dupilumab displayed that this drug appears to decrease the activity of HSD3B1. Both these pieces of evidence indicate that IL-4 and IL-13 trigger this gene activity.
To examine the effect of the gene on sebum output, the scientists altered the activity of HSD3B1 in sebocytes cultured in Petri dishes. They observed that when the gene was made less active, the levels of sex hormones reduced, but the skin sebum production heightened.
The reverse can also be held true—the higher the gene activity, the greater is the number of sex hormones and reduced sebum. The scientists made equivalent observations in a mouse model of AD, with sex hormone production reducing the production of skin lipids.
Altogether, Dr. Harris-Tryon put forth that these observations indicate that HSD3B1 can be a novel target for combating AD and possibly other forms of eczema.
Changing the output of this gene could eventually offer a way to treat AD that’s completely different from any treatment that currently exists.”
Tamia Harris-Tryon MD, PhD, Study Corresponding Author and Assistant Professor, Dermatology and Immunology, UT Southwestern Medical Center
Source:
Journal reference:
Zhang, C., et al. (2021) Interleukins 4 and 13 drive lipid abnormalities in skin cells through regulation of sex steroid hormone synthesis. Proceedings of the National Academy of Sciences of the United States of America. doi.org/10.1073/pnas.2100749118.