Ghent University’s professor Braeckmans concentrated on a technique for the safe engineering of therapeutic cells with photothermal nanofibers for the past decade. The research published in Nature Nanotechnology sheds light on the formation of these biocompatible photothermal nanofibers.
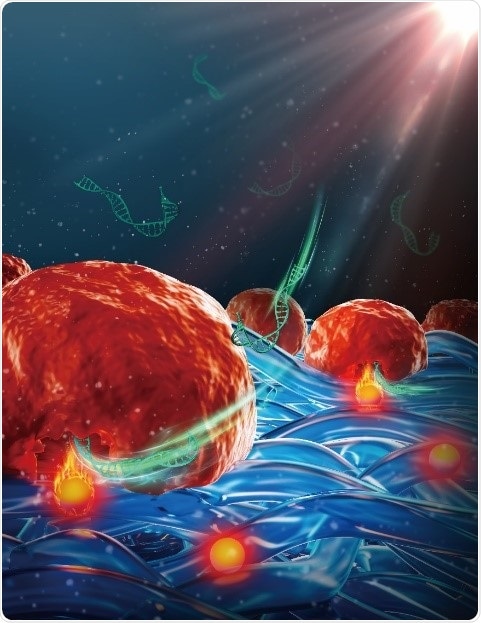
Cells on photothermal nanofibers become permeabilized and transfected upon laser irradiation. Image Credit: Ghent University
It also provides insight on how during laser irradiation, cells that come in contact with those nanofibers become permeabilized and can be transfected with various effector molecules, like siRNA and CRISPR/Cas9 ribonucleoprotein complexes.
Professor Braeckmans and his group showed that cells, like human T cells and embryonic stem cells, transfected with such nanofibers are in great health and maintain their therapeutic functionality.
New basis for cell-based therapies
Cell-based therapies make up a newer form of treatment where genetically modified cells are injected into patients to evade or treat illnesses. A renowned example is employing a cancer patient’s immune cells—isolated, genetically modified, and grown in a laboratory environment—reinfused into the patient to kill tumor cells.
Genetic modification of cells relies on intracellular delivery techniques which mostly struggle with getting adequate efficiency while having minimal effect on the cell’s health and functioning.
Nanoparticle-sensitized photoporation is specifically promising in this regard as it offers high throughput, greater efficacy, and less toxicity. It depends on the use of light-responsive nanoparticles, like gold nanoparticles (NPs), which can create explosive nanobubbles upon pulsed laser irradiation.
Those tiny explosions can produce small pores in cell membranes, permitting external effector molecules supplemented in the cell medium to enter cells. Yet, translation of nanoparticle-sensitized photoporation to clinical applications is obstructed as cells were in contact with (non-degradable) nanoparticles, posing regulatory and toxicological concerns.
Hence, there is a need for a novel approach that maintains the advantage of nanoparticle-sensitized photoporation at the same time preventing direct contact of nanoparticles and cells. Professor Braeckmans and his group embedded photothermal iron-oxide nanoparticles (IONPs) into biocompatible polymeric nanofibers, created by electrospinning.
IONPs are economical and have a wide light absorption spectrum while polycaprolacton (PCL) is a biocompatible polymer commonly utilized in biomedical applications.
The researchers demonstrated that both adherent and suspension cells can be transfected effectively and safely with a range of macromolecules following irradiation with nanosecond laser pulses.
The scientists carried out elemental analysis via inductively coupled plasma—tandem mass spectrometry (ICP-MS/MS) and substantiated that IONPs are safely enclosed in the nanofibers after laser irradiation. This ensures that the treated cells are free from direct exposure to nanoparticles.
Numerical simulations on heat transfer from fiber-embedded IONPs to nearby cells were carried out to comprehend the influence of laser pulse fluence, IONP distribution, and aggregation state on cell membrane permeability.
The researchers proved experimentally that photoporation with photothermal nanofibers can be used effectively to deliver functional biological molecules like CRISP-Cas9 ribonucleoproteins (RNPs) or siRNA, to both adherent and suspension cells, including primary human T cells and human embryonic stem cell (hESC).
They also performed a comparison with advanced electroporation as a benchmark. Electroporated cells suffered phenotypical changes and changes in functionality, while photoporated cells preserved their capability to proliferate—in the case of CAR-T cells, to destroy tumor cells.
Eventually, PEN photoporation was employed to transfect CAR-T cells with siRNA targeting the PD1 receptor, an eminent immune checkpoint inhibitor. siPD1 treated cells were affirmed to have improved efficiency towards destroying tumors in vivo.
It is demonstrated that photoporation coupled with photothermal nanofibers allows safe and effective intracellular delivery of a wide range of effector molecules and different types of cells without contact with toxic photothermal nanoparticles.
We believe this is an important step towards the use of photoporation for safe and efficient production of gene-modified cell therapies.”
Kevin Braeckmans, Professor, Ghent University
Source:
Journal reference:
Xiong, R., et al. (2021) Photothermal nanofibres enable safe engineering of therapeutic cells. Nature Nanotechnology. doi.org/10.1038/s41565-021-00976-3.