Around 3%–10% of the individuals infected by the SARS-CoV-2 experience moderate to severe disease. In such cases, the immune system overreacts to the virus, inducing an aberrant innate immune response marked by intravascular blood clotting, systemic inflammation, and damage to the cardiovascular system.
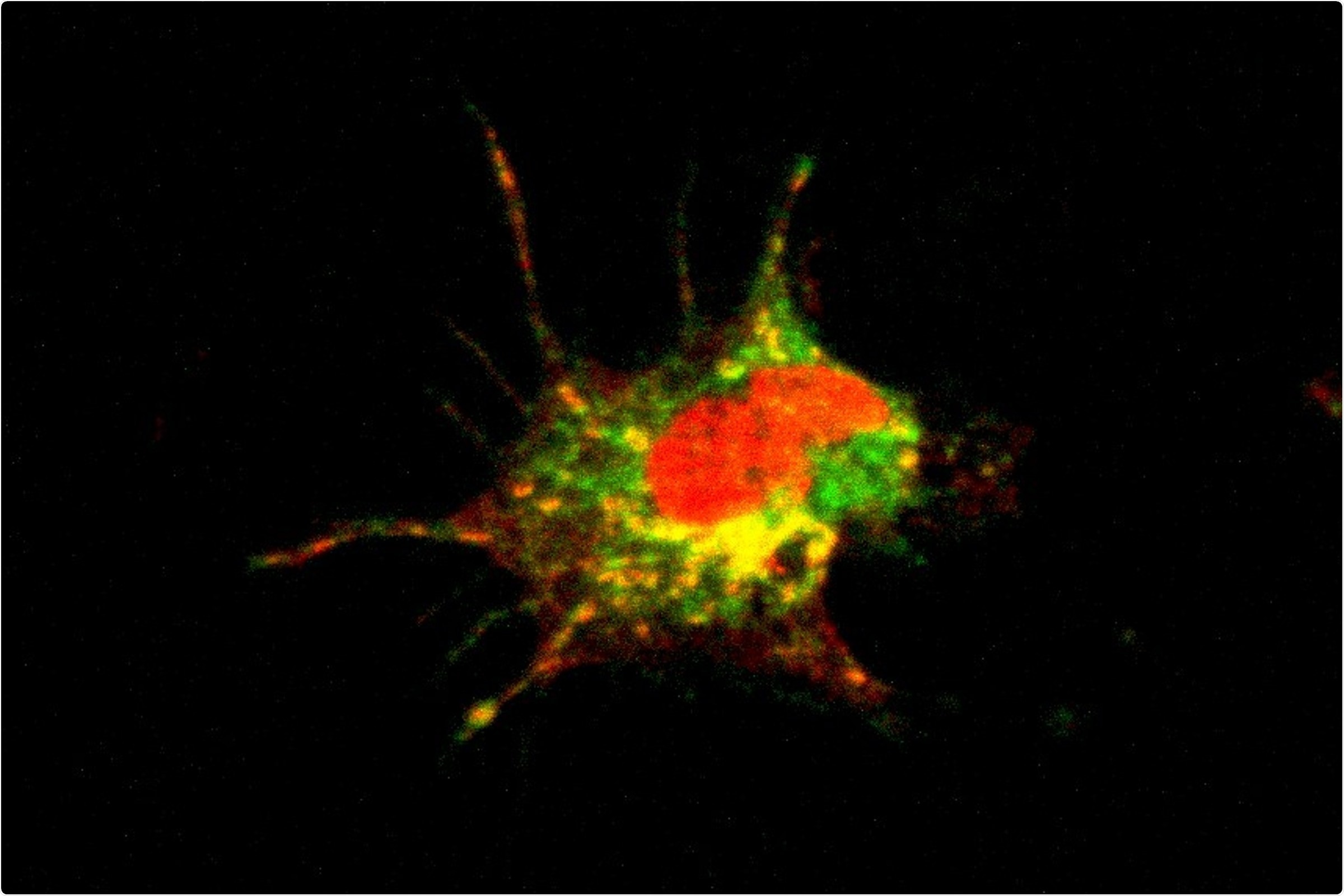
Dendritic cell. Image Credit: © D. Dudziak.
A group headed by the immunology professor Anne Krug at LMU’s Biomedical Center (BMC), including scientists from the BMC and the LMU Medical Center, performed extensive research on this phenomenon and unraveled earlier unknown effects of the virus on the immune system.
The researchers state that after infection with SARS-CoV-2, there occurs a decline in the number of dendritic cells in the circulation, and also the functionality of the remaining fraction is damaged. The researchers affirm that this makes patients more vulnerable to secondary infections during, and soon after recovery from COVID-19 infections. The research was published in the journal PLOS Pathogens.
Dendritic cells (DCs) are the ones that commence immune responses against invasive pathogens by activating helper T cells, which triggers B cells to produce antibodies against the pathogen. Krug and co-workers wanted to analyze the impacts of moderate to severe coronavirus infection on this process. They examined blood samples collected from 65 COVID-19 patients treated at the LMU Medical Center.
The researchers discovered that there are fewer DCs in those samples when compared to the blood of healthy individuals. Moreover, the DCs isolated from the patients displayed a decreased capability to activate T cells.
We had actually expected that DCs isolated from patients infected with SARS-CoV-2 would activate T cells more potently than DCs obtained from healthy donors. However, we discovered that, in the course of the disease, the proteins present on the surface of the DCs in patients’ blood were altered in a way that made them more likely to inhibit T cell responses.”
Anne Krug, Immunology Professor, Biomedical Center, Ludwig Maximilian University of Munich
Despite this, by day 15, after diagnosis, 90% of the patients produced antibodies against the SARS-CoV-2 spike protein, and most of them also triggered a T cell response—characteristic of a powerful immune reaction against the virus.
So, the drop in the numbers and reduced functionality of DCs does not seem to have a negative impact on the immune response to the coronavirus itself.”
Anne Krug, Immunology Professor, Biomedical Center, Ludwig Maximilian University of Munich
Possibly impaired immune response
The researcher is certain that the decreased number and altered function of DCs are vital. It is likely that this might be the reason why the immune system reacts less strongly than anticipated to other viral or bacterial infections post recovery from COVID-19. However, this possibility requires further clinical examination.
Krug has numerous hypotheses to provide for the question, what might be the reason for the reduction of DCs in the blood and the reduced capability to trigger T cells? Krug states that it could represent a suitable regulatory process. COVID-19 is mostly linked to robust inflammation reactions and hence the phenomenon may be part of an attempt to downregulate inflammatory processes.
Dendritic cells may move from the blood to the site of inflammation, for instance, the lung, which explains the decrease in the count of DCs in circulation.
However, we also found that the regeneration of dendritic cells is delayed.”
Anne Krug, Immunology Professor, Biomedical Center, Ludwig Maximilian University of Munich
The researchers assume that this phenomenon can diminish the capability of patients to produce effective immune responses to other pathogens during and immediately after a symptomatic COVID-19 infection. The researchers further intend to analyze this issue in an effort to find out if the impacts of SARS-CoV-2 on DCs perform a role in long-term COVID.
Source:
Journal reference:
Winheim, E., et al. (2021) Impaired function and delayed regeneration of dendritic cells in COVID-19. PLoS Pathogens. doi.org/10.1371/journal.ppat.1009742.