Cancer cells should avoid the immune system to grow and spread. Researchers from the Brigham and Women’s Hospital and MIT utilized the power of nanotechnology to identify a novel means that cancer cells use to disarm their would-be cellular attackers.
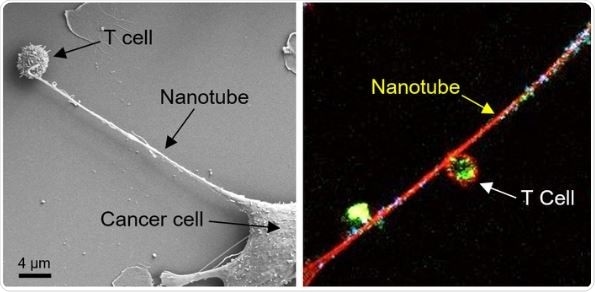
Left: Field emission scanning electron microscopy (FESEM) image shows the formation of a nanotube between a breast cancer cell and an immune cell. Right: Confocal microscopy image shows mitochondria (labeled with green fluorescence dye) traveling from a T cell to a cancer cell through the intercellular nanotube. DNA in the mitochondria was labeled with blue dye. Image Credit: Nature Nanotechnology.
Cancer cells by stretching out their nanoscale tentacles reach an immune cell and remove its powerpack. Taking out the mitochondria of the immune cell powers up the cancer cell and exhausts the immune cell. The findings could guide to new targets for the creation next generation of immunotherapy against cancer. The observations are published in the Nature Nanotechnology journal.
Cancer kills when the immune system is suppressed and cancer cells are able to metastasize, and it appears that nanotubes can help them do both. This is a completely new mechanism by which cancer cells evade the immune system and it gives us a new target to go after.”
Shiladitya Sengupta PhD, Study Corresponding Author and Co-Director, Center for Engineered Therapeutics, Brigham and Women’s Hospital
To analyze the interaction between cancer cells and immune cells at the nanoscale level, Sengupta and co-workers carried out experiments where they co-cultured breast cancer cells and immune cells, like T cells.
Under a field-emission scanning electron microscopy, the researchers found a glimpse of something peculiar—cancer cells and immune cells were seen to be physically linked by tiny tendrils, with widths in the range of 100 nm–1000 nm (A human hair is approximately 80,000 nm–100,000 nm).
In certain cases, the nanotubes came together to form thicker tubes. The researchers later stained mitochondria—the organelle which provides energy for cells—of the T cells with a fluorescent dye and observed that bright green mitochondria were drawn out of the immune cells through the nanotubes into the cancer cells.
By carefully preserving the cell culture condition and observing intracellular structures, we saw these delicate nanotubes and they were stealing the immune cells’ energy source. It was very exciting because this kind of behavior had never been observed before in cancer cells. This was a tough project as the nanotubes are fragile and we had to handle the cells very gently to not break them.”
Hae Lin Jang PhD, Study Co-Corresponding Author and Principal Investigator, Center for Engineered Therapeutics, Brigham and Women’s Hospital
The scientist then investigated what happens when the hijacking of mitochondria was prevented. They introduced an inhibitor of nanotube development into mouse models used for analyzing lung cancer and breast cancer and observed a substantial reduction in tumor growth.
One of the goals in cancer immunotherapy is to find combinations of therapies that can improve outcomes. Based on our observations, there is evidence that an inhibitor of nanotube formation could be combined with cancer immunotherapies and tested to see if it can improve outcomes for patients.”
Tanmoy Saha PhD, Study Lead Author and Postdoctoral Researcher, Center for Engineered Therapeutics, Brigham and Women’s Hospital
Source:
Journal reference:
Saha, T., et al. (2021) Intercellular nanotubes mediate mitochondrial trafficking between cancer and immune cells. Nature Nanotechnology. doi.org/10.1038/s41565-021-01000-4.