Reviewed by Danielle Ellis, B.Sc.Jun 10 2022
The interferon-gamma receptor (IFNgR) signaling pathway has been identified to be crucial for the vulnerability of glioblastoma tumors to death by CAR T-cell immunotherapy, according to researchers at Massachusetts General Hospital (MGH).
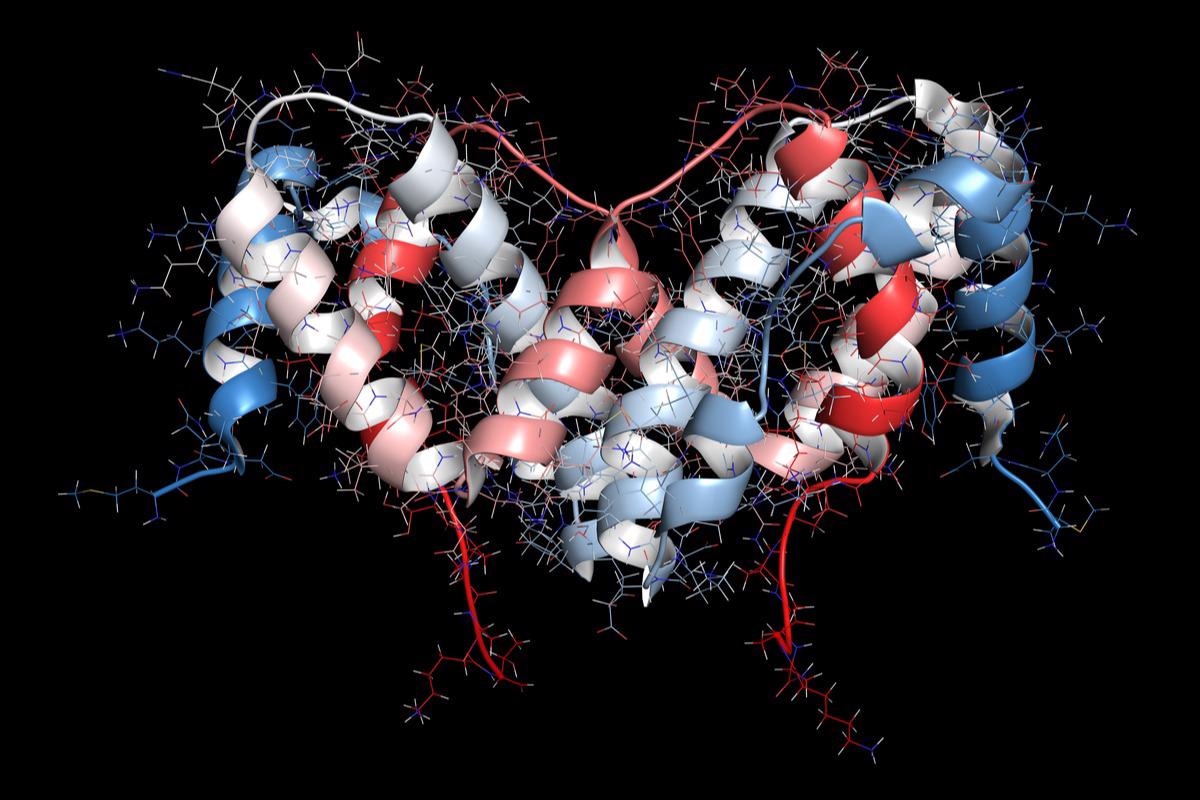
Image Credit: StudioMolekuul/Shtterstock.com
The same thing happened with other solid tumors. This finding could help to explain why liquid and solid tumors respond to CAR T-cell therapy so variably. The findings were reported in the journal Nature.
A chimeric antigen receptor (CAR) is a synthetic molecule that instructs the immune system’s T cells to recognize and adhere to a target, or antigen. CARs can detect targets on the surface of tumor cells. While CAR therapy has revolutionized the treatment of hematologic diseases such as leukemia and lymphoma, it has yet to achieve the same level of success in solid tumors.
Scientists headed by Marcela Maus, MD, PhD, director of the Cellular Immunotherapy Program at the Mass General Hospital Cancer Center, created a genome-wide CRISPR knockout screen in glioblastoma to find resistance pathways in solid tumors.
With a CRISPR screen, we were able to interrogate the entire genome in a pooled format in a completely unbiased manner, instead of looking for one or two genes of interest at a time.”
Rebecca Larson PhD, Study First Author, Massachusetts General Hospital Cancer Center
This allowed scientists to discover which genes were deleted and to figure out how solid tumors avoid CAR T-cell therapy by using resistance mechanisms. They used a CAR to provide selective pressure to each barcoded cell in the screen in their work.
We then sequenced the cells and could see which tumor cells were alive afterward telling us which genes were knocked out.”
Rebecca Larson PhD, Study First Author, Massachusetts General Hospital Cancer Center
When Larson and colleagues ran the screen on a variety of glioblastoma cell lines, such as those generated from patients, they discovered that knocking out genes in the interferon gamma-signaling pathway rendered the cells resistant to CAR T-cell killing.
“That means those interferon gamma-related genes are necessary for the tumor to die in the face of a CAR, something we had not known before and that we did not expect,” adds Larson.
In knockout mice models, the same resistance pattern was discovered in vivo. Resistance to CAR T-cell therapy was found to be caused by the loss of interferon-gamma pathway genes in various solid tumor cell lines, particularly pancreatic, ovarian, and lung cell lines.
“We found that CAR T-cells did not bind to glioblastoma cells lacking interferon-gamma signaling,” Larson went on to say, that while interferon-gamma does not directly kill cancer, it does make tumor cells stickier. “That way, the CAR T-cell can bind to it better and eliminate the cancer cell.”
The interferon-gamma pathway, on the other hand, did not play a role in the sensitivity of leukemia, lymphoma, or multiple myeloma to CAR T-cell therapy, according to the scientists.
The fact that we can see how solid and liquid tumors are responding to CAR T-cell therapy in different ways is very informative for how we design a future therapy.”
Rebecca Larson PhD, Study First Author, Massachusetts General Hospital Cancer Center
According to Maus, moving forward, this revelation provides researchers with a clinical chance on two fronts. To begin, improving T-cell/tumor cell interactions by aiming at the interferon-gamma pathway may result in better responses to CAR T-cell therapy in solid tumors. Furthermore, blocking this pathway in liquid tumors may significantly minimize the well-known cytokine release syndrome toxicity of CAR T-cell therapies.
“Even though CAR T-cell treatment can in some cases be amazingly effective with more than 40% cure rates in some liquid tumors, toxicity is a real concern,” she adds. “Tamping down the interferon-gamma in these cancers might keep the efficacy but reduce the rollercoaster of toxicity.”
Source:
Journal reference:
Larson, R. C., et al. (2022) CAR T cell killing requires the IFNγR pathway in solid but not liquid tumors. Nature. doi.org/10.1038/s41586-022-04585-5.