Heart damage is prevalent in COVID-19 patients, leading many to doubt how the virus impacts the heart.
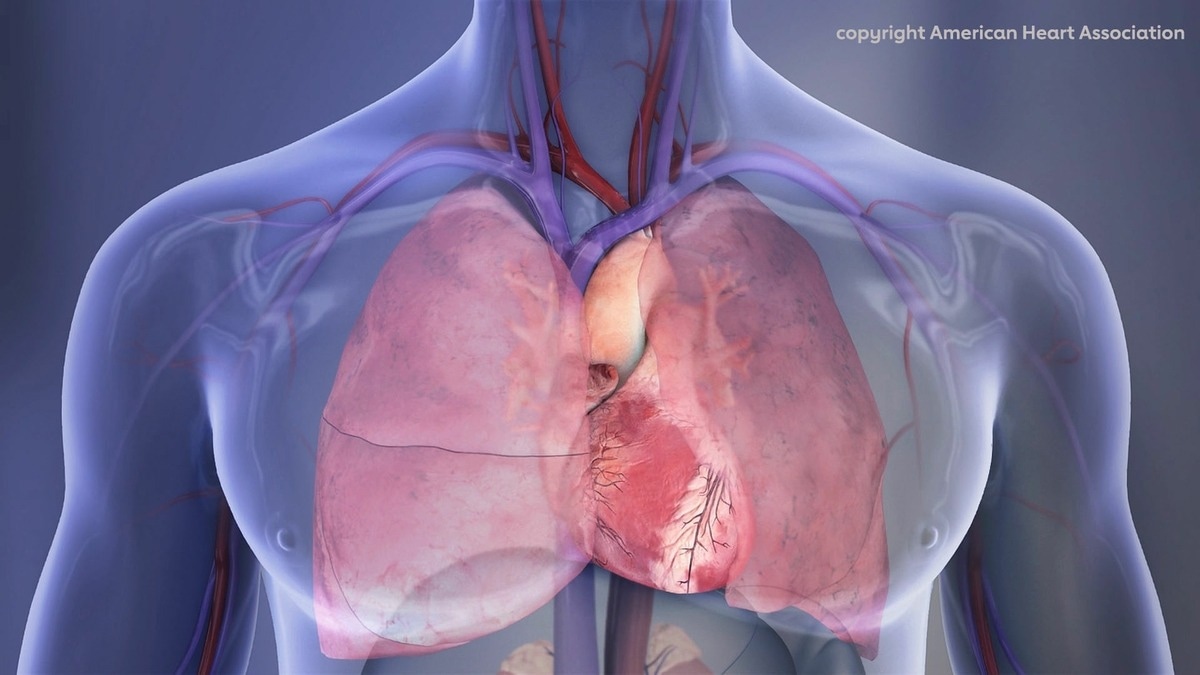 Human Chest Cavity illustration: Right lung, left lung, heart. Image Credit: American Heart Association
Human Chest Cavity illustration: Right lung, left lung, heart. Image Credit: American Heart Association
According to early studies displayed at the American Heart Association’s Basic Cardiovascular Sciences Scientific Sessions 2022, the spike protein from the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus can cause heart muscle injury through the inflammatory phase.
The meeting, which takes place in Chicago from July 25th to 28th, 2022, provides the most recent research in basic and translational cardiovascular science.
The spike protein is located on the surface of the virus that causes COVID-19 and SARS-CoV-2. Spike proteins bind to angiotensin-converting enzyme 2 (ACE2) receptors on target cells.
The spike protein makes it easier for viruses to enter healthy cells, which would be the first process of infection. In addition to contaminating the lungs, the virus can spread to other organs, causing further damage, severe infection, and, in some cases, death.
It’s already known from the clinical side that COVID-19 infection can induce heart injury, however, what we don’t know is the mechanistic details of how this occurs. What we suspect is that the spike protein has unknown pathological roles. Our data show that the spike protein from SARS-CoV-2 causes heart muscle damage. That’s why it’s important to get vaccinated and prevent this disease.”
Zhiqiang Lin, PhD., Study Lead Author and Assistant Professor, Masonic Medical Research Institute
“Host natural immunity is the first line of defense against pathogen invasion, and heart muscle cells have their natural immune machinery. Activation of the body’s immune response is essential for fighting against virus infection; however, this may also impair heart muscle cell function and even lead to cell death and heart failure,” Lin said.
The researchers wanted to see if the SARS-CoV-2 spike protein triggered the body’s natural immune reaction in heart muscle cells. Although its spike protein also utilizes ACE2 to mediate virus entry, HCoV-NL63 is a coronavirus that infects the respiratory system without provoking cardiac injury.
They evaluated the possibility of the SARS-CoV-2 spike protein and the NL63 spike protein causing heart disease. The SARS-CoV-2 spike protein powered up the natural immune response in heart muscle cells, causing damage to the heart, but the NL63 spike protein did not.
“The fact that the SARS-CoV-2 spike protein is activating the natural immune response may explain the high virulence compared to the other coronaviruses,” Lin said. “The TLR4 signaling is the major pathway that activates the body’s natural immune response, and the SARS-CoV-2 spike protein activates TLR4, not the regular flu spike protein.”
Scientists cloned the SARS-CoV-2 spike protein and the NL63 spike protein into the AAV9 viral vector to analyze the effects of the SARS-CoV-2 spike protein on the heart. To stimulate the spike protein in heart muscle cells, the AAV9 viral vector was produced in lab mice.
They discovered that the SARS-CoV-2 spike protein, rather than the NL63 spike protein, was mediated by AAV9 and caused heart failure, hypertrophic remodeling (enlargement), and cardiac inflammation.
In lab tests on heart cells cultured in dishes, scientists found that the SARS-CoV-2 spike protein caused heart muscle cells to grow significantly larger than cells without either spike proteins.
“We found direct evidence that the SARS-CoV-2 spike protein is toxic to heart muscle cells,” Lin said.
During this investigation, researchers also looked at a heart biopsy from a dead patient who had COVID-19 inflammation. They discovered the SARS-CoV-2 spike protein and the TLR4 protein in heart muscle cells as well as other cell types. In comparison, these two proteins were not found in a proper human heart biopsy.
That means once the heart is infected with SARS-CoV-2, it will activate the TLR4 signaling. Besides directly damaging the heart muscle cells, the spike protein itself is very inflammatory and may cause systemic inflammation that indirectly causes heart problems.”
Zhiqiang Lin, PhD., Study Lead Author and Assistant Professor, Masonic Medical Research Institute
ACE2 is a vital enzyme in the regulation of blood pressure. SARS-CoV-2 infection may affect ACE2 function, resulting in an increase in blood pressure and, as a result, heart damage. SARS-CoV-2 may also harm the heart via unidentified pathways.
“Our study provides two pieces of evidence that the SARS-CoV-2 spike protein does not need ACE2 to injure the heart. First, we found that the SARS-CoV-2 spike protein injured the heart of lab mice. Different from ACE2 in humans, ACE2 in mice does not interact with SARS-CoV-2 spike protein, therefore, SARS-CoV-2 spike protein did not injure the heart by directly disrupting ACE2 function,” Lin said.
“Second, although both the SARS-CoV-2 and NL63 coronaviruses use ACE2 as a receptor to infect cells, only the SARS-CoV-2 spike protein interacted with TLR4 and inflamed the heart muscle cells. Therefore, our study presents a novel, ACE2-independent pathological role of the SARS-CoV-2 spike protein,” Lin added.
This study is the first step in establishing whether the SARS-CoV-2 spike protein has any effect on the heart. The scientists will now look into how SARS-CoV-2 spike proteins cause heart inflammation.
There are two possibilities: the virus spike protein is produced in virus-infected heart muscle cells, straightforwardly activating inflammation, and the virus spike protein is shed into the bloodstream, where circulating SARS-CoV-2 spike proteins damage the heart.