More than 10,000 different Mycobacterium tuberculosis bacteria isolated from 23 different countries were subjected to a thorough investigation, which uncovered new genes linked to resistance to 13 first- and second-line novel and repurposed medicines.
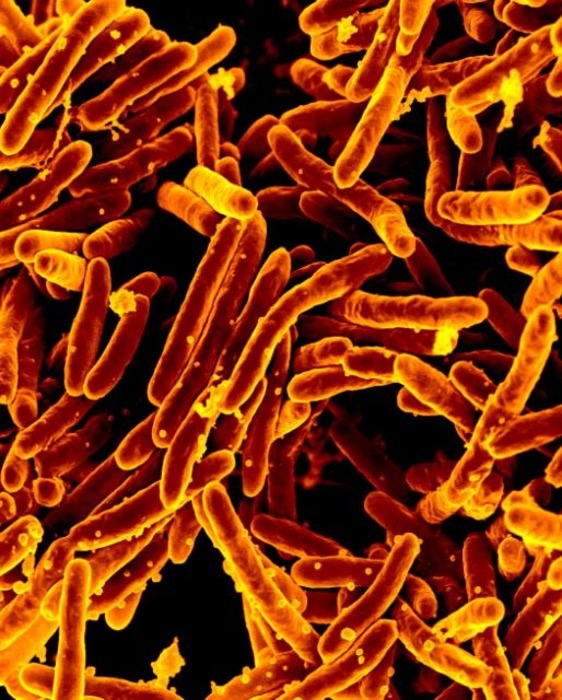 Mycobacterium tuberculosis Bacteria, the Cause of TB. Image Credit: NIAID, Flickr (CC-BY 2.0, https://creativecommons.org/licenses/by/2.0/)
Mycobacterium tuberculosis Bacteria, the Cause of TB. Image Credit: NIAID, Flickr (CC-BY 2.0, https://creativecommons.org/licenses/by/2.0/)
Two new studies that are to be published on August 11th, 2022, in the open-access journal PLOS Biology highlight the work done by the Comprehensive Resistance Prediction for Tuberculosis: an International Consortium (CRyPTIC).
Around 85% of persons with TB can be successfully treated with a six-month medication regimen; TB is a curable and preventable disease. Considering this, TB continues to raise a concern and has killed people more recently than any other infectious disease. Improved monitoring of resistant strains and the creation of novel treatments both depend on a greater understanding of the M. tuberculosis variations that cause antibiotic resistance.
The researchers described how they put together an open-access data compendium of 12,289 M. tuberculosis isolates that had been processed at CRyPTIC partner laboratories all around the world in the first new paper.
Each isolate was sequenced before being tested using a high-throughput grid and 13 antimicrobials at various doses. About 6,814 of the samples in the compendium were drug-resistant to at least one degree, including 4,685 samples that were also resistant to more than one drug or the first-line antibiotic rifampicin.
The consortium published its findings from a genome-wide association study (GWAS) that used data on 10,228 M. tuberculosis isolates in the second paper. The team found uncatalogued variations for each of the 13 medicines that significantly increased the minimum inhibitory concentration—the lowest concentration at which an antibiotic can stop M. tuberculosis from proliferating.
Instead of using a binary outcome of resistant-or-not-resistant, analyzing this concentration permitted the discovery of variants that only slightly alter the response to antibiotics and can be remedied by raising drug dosage. The effect magnitude and variations within these particular genes were discussed in further detail. The researchers chose the 20 most important genes that give resistance to each medication.
“Our study demonstrates the ability of global partnerships to substantially improve our knowledge of genetic variants associated with antimicrobial resistance in M. tuberculosis,” the authors note.
Together, the publications provide a foundation for further research on the disease in addition to identifying individual genes that may be followed up on to comprehend the M. tuberculosis resistance landscape.
“The compendium is not designed for measuring prevalence or estimating ‘real-world’ error rates of resistance prediction tools; rather it serves as a resource to accelerate antimicrobial resistance diagnostic development by enriching mutation catalogs for [whole genome sequencing] resistance prediction, improving our understanding of the genetic mechanisms of resistance, and identifying important diagnostic gaps and drug resistance patterns,” authors say.
“The data compendium is fully open-source and it is hoped that it will facilitate and inspire future research for years to come.”
Source:
Journal reference:
Crook, D. W., et al. (2022) A data compendium associating the genomes of 12,289 Mycobacterium tuberculosis isolates with quantitative resistance phenotypes to 13 antibiotics. PLOS Biology. doi.org/10.1371/journal.pbio.3001721.