The University of Michigan’s Rogel Cancer Center researchers discovered a mechanism that explains why a subset of patients’ tumors grows rather than shrink when treated with immunotherapy.
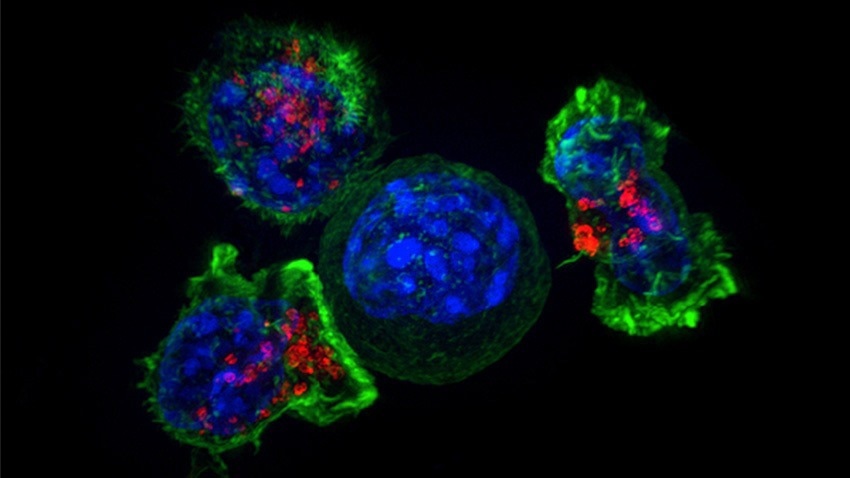 Patients who were not deriving any benefit from immunotherapy had a similar CD8+T cell infiltration as those patients who benefited tremendously. Image Credit: NCI—Visuals Online
Patients who were not deriving any benefit from immunotherapy had a similar CD8+T cell infiltration as those patients who benefited tremendously. Image Credit: NCI—Visuals Online
Immunotherapy has made significant advances in cancer therapy; however, it is not efficacious for all patients. It can even end up causing tumors to “hyperprogress” in some cases.
Weiping Zou, MD, PhD, and Michael D. Green, MD, PhD of Rogel used tumor samples from patients in addition to mouse models to examine the molecular pathways involved when immunotherapy worsens, rather than slows, disease progression. The findings were published in Cancer Cell.
Researchers discovered that tumors with hyperprogression after immunotherapy had increased levels of fibroblast growth factor 2, or FGF2, and beta-catenin signaling. Furthermore, the mouse models demonstrated that the gene signaling interferon γ, which is derived from CD8+ T cells, causes hyperprogression disease by rewiring the tumors’ metabolic pathways.
The researchers predicted that patients with hyperprogression disease would have fewer immune cells, such as CD8+T cells and the interferon γ gene signature.
But the patients who weren’t deriving any benefit from immunotherapy had a similar CD8+T cell infiltration as those patients who benefited tremendously.”
Michael D. Green, Study Co-Lead Author and Assistant Professor, Radiation Oncology, Rogel Cancer Center, University of Michigan
The researchers hypothesized that the patients’ hyperprogression disease was caused by the immunotherapy itself, but they needed to examine this controversial finding further in experimental mouse models.
We really wanted to understand if there are biomarkers that can predict, before the patient receives immunotherapy if they will develop hyperprogression disease from the treatment.”
Weiping Zou, Study Co-Lead Author and Director, Center of Excellence for Cancer Immunology and Immunotherapy
The solution lay at the intersections of immunogenic, metabolic, and oncogenic pathways. In preclinical models, the researchers discovered that targeting the gene signaling axis of interferon γ, FGF2, and beta-catenin prevents hyperprogression.
These findings are provocative. We usually think that immunotherapy is beneficial, but now we have evidence that for a subset of patients, it’s not only not beneficial but potentially harmful for patients. If we can get to the stage of being able to identify those patients who shouldn’t receive treatment beforehand, that will be very important.”
Weiping Zou, Study Co-Lead Author and Director, Center of Excellence for Cancer Immunology and Immunotherapy
The study was collaborative, involving associates from all across Rogel, including Arul Chinnaiyan, MD, PhD, SP Hicks Endowed Professor of Pathology and Director of the Michigan Center for Translational Pathology, who provided input from a molecular pathology and cancer genomics viewpoint.
“This is an impressive study beginning in the clinic, with hypotheses generated from cancer patients treated with immunotherapy, and goes to the bench by mechanistically investigating these hypotheses in pre-clinical models. This is a stellar example of how basic research can teach us about how cancer patients have varied responses to immunotherapy,” stated Chinnaiyan.
To target this gene signaling axis in patients, more clinical research is necessary.
Source:
Journal reference:
Li, G., et al. (2023) Intersection of immune and oncometabolic pathways drives cancer hyperprogression during immunotherapy. Cancer Cell. doi.org/10.1016/j.ccell.2022.12.008.