According to a new study performed at the Earlham Institute and Quadram Institute in Norwich, the community of microbes living in and on human bodies might be serving as a reservoir for antibiotic resistance.
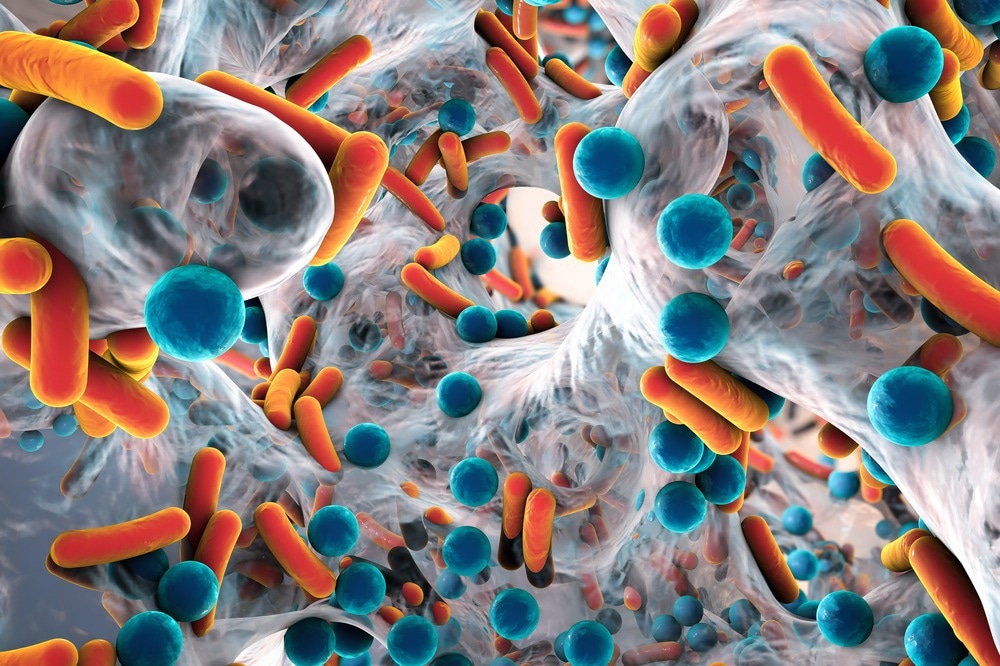
Image Credit: Kateryna Kon/Shutterstock.com
The usage of antibiotics results in so-called “collateral damage” to the microbiome, thereby gradually increasing the number of resistance genes that are being passed back and forth between strains present in the microbiome.
Also, the study findings indicate such genes tend to spread so easily via a population that, irrespective of their health and habits, the number of resistance genes present in the gut is heavily impacted by national trends present in antibiotic consumption.
Among human pathogens, the increase of antimicrobial resistance (AMR) is extensively seen as one of the most detrimental threats to global health in the forthcoming decades. Already, AMR is thought to be contributing to tens of thousands of deaths in Europe annually.
Normally, tracking the birth and spread of genes that assist such pathogens to ignore antibiotics have been restricted to samples that have been taken from infected individuals. But most of the microbes living in the human body are not pathogenic.
The human microbiome is known to be a complicated and dynamic community of millions of species of microbes, mainly living in the gut and coexisting with humans. Microbiomes tend to play a significant role in health and disease, along with the gut microbiome familiar to help with the digestion of food and also the development of the immune system.
Even a healthy individual, who hasn’t taken antibiotics recently, is constantly bombarded by microbes from people or even pets they interact with, which leads to resistance genes becoming embedded in their microbiota. If they exist in a population with a heavy burden of antibiotic consumption, it leads to more resistance genes in their microbiome.”
Chris Quince, Study Author of Research, Professor, Earlham Institute
Quince is also a professor at Quadram Institute.
To better comprehend the effect of antimicrobials on the gut microbiome, scientists at the Earlham Institute and Quadram Institute in Norwich, collectively with collaborators in the Republic of Korea, examined more than 3,000 gut microbiome samples, gathered from healthy individuals throughout 14 countries.
Further, they made a comparison of the resistance genes determined in samples to those discovered in large genome collections to comprehend the movement of AMR genes between pathogen and microbe species.
We deliberately focussed on samples from healthy people, or at least those we could be confident weren’t taking antibiotics. We needed to see the gene profile in the gut microbiome without the influence of any antimicrobials.”
Chris Quince, Study Author of Research, Professor, Earlham Institute
By making a comparison of the data with the Comprehensive Antibiotic Resistance Database, the researchers cautiously cataloged and recorded the number of antimicrobial resistance genes discovered in the samples. The database is known as a public health resource where resistance genes have been documented.
The team determined a median of 16 AMR genes per stool sample examined. Also, they discovered that the median number of genes altered across the 14 countries for which there was data with the researchers.
For instance, they noted a five-fold difference in median resistance levels between the highest in Spain and the lowest in the Netherlands.
With the help of World Health Organization and ResistanceMap data, the research group was able to display a powerful correlation between the frequency of resistance genes present in a country and as well as national antibiotic consumption levels.
Quince stated, “We found that, in countries where antibiotics are taken more regularly, their populations also have higher numbers of resistance genes in their gut microbiome.”
The cause for this collateral damage to turn out to be such a major issue is that microbes are continuously sharing genes. Also, referred to as horizontal gene transfer, this process aids AMR genes to spread back and forth between the species.
Our bodies are continually importing and exporting microbes and pathogen strains. These strains are themselves passing genes back and forth, which means the challenge of AMR has to be tackled at both the micro and macro level.”
Chris Quince, Study Author of Research, Professor, Earlham Institute
Quince stated, “Given our complex relationship with microbes, we need to do more research to understand how we maximize the benefits and minimize the risks when it comes to guiding treatment decisions and developing new medicines.”
Professor Falk Hildebrand, a research author at the Quadram Institute and Earlham Institute, stated, “We’ve known for some years that antimicrobial resistance genes can spread incredibly fast between gut bacteria.
Hildebrand added, “This study is so important because it can, for the first time, quantify the impact national antibiotic usage has on our commensal bacteria, as well as giving us insights into the common types of resistance we can expect to evolve.”
The scientists plan to perform additional research and encourage others to examine the relationship in more countries and further inform public health strategies.
The study was financially supported by UKRI-Biotechnology and Biological Sciences Research Council, UKRI-Natural Environment Research Council, and the European Research Council.
Source:
Journal reference:
Lee, K., et al. (2023) Population-level impacts of antibiotic usage on the human gut microbiome. Nature Communications. doi.org/10.1038/s41467-023-36633-7.