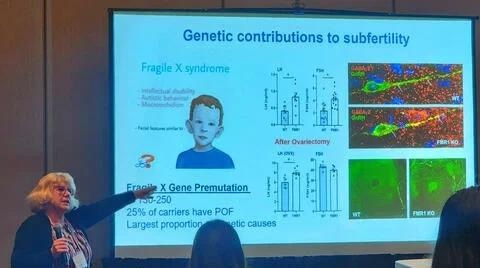
The biological foundations of a reproductive disease caused by a DNA mutation have been discovered by a University of California, Riverside study. Fragile X Syndrome, a major genetic contributor to cerebral impairment and autism, is also caused by this gene mutation.
 Djurdjica Coss is a professor of biomedical sciences at UC Riverside. Image Credit: UCR/Coss lab
Djurdjica Coss is a professor of biomedical sciences at UC Riverside. Image Credit: UCR/Coss lab
The Fragile X messenger ribonucleoprotein 1 gene, or FMR1, was discovered to contribute to premature ovarian failure, or POF, as a result of alterations in the neurons that control reproduction in the brain and ovaries. The mutation has been linked to early infertility because there is a 25-fold higher chance of POF, but the causes of this association were not obvious.
About 10% of women experience POF, which is the gravest form of premature ovarian aging and is characterized by early menopause and early ovarian follicle loss. Women who put off having children are more likely to experience infertility, including when the FMR1 gene is mutated.
In the last two or three decades, the median age of first-time mothers in the U.S. and Europe has steadily increased. Moreover, premature menopause causes not only early infertility, but also increased risk of cardiovascular disease and osteoporosis. It is important, therefore, to understand the reasons behind these reproductive disorders and eventually find treatments. Such research can also help better advise women at risk on when to have a child and how to monitor their health outcomes.”
Djurdjica Coss, Professor, Biomedical Sciences, School of Medicine, University of California, Riverside
According to the Centers for Disease Control and Prevention, 19% of heterosexual couples in the United States are infertile and require assisted reproductive technology, which is often prohibitively expensive for many couples.
Coss noted that earlier studies of the FMR1-mediated reproductive diseases were purely endocrine in nature, focusing on changes in hormone levels and the operation of endocrine cells in the ovaries that generate the hormones.
Coss added, “We took a different approach. Since the FMR1 gene is highly abundant in neurons, we postulated that neurons that regulate reproduction are affected by the FMR1 mutation, which in turn causes increases in hormone levels. Indeed, we found higher stimulation of neurons in the hypothalamus that regulate reproduction as well as more neurons in the ovaries that contribute to ovarian hormone synthesis.”
Coss and her colleagues replicated the situation in individuals with a mutation in the FMR1 gene using transgenic mice lacking the gene for their study. They first discovered that the symptoms seen in women with an FMR1 mutation are mimicked by this mouse model.
The reproduction-regulating neurons in the ovaries and the brain of these mice were then compared with those in normal mice.
They discovered that in young transgenic female mice that subsequently ceased reproducing early, the altered function of these neurons caused a more rapid secretion of hormones. To examine the impact of the FMR1 mutation on just the brain’s neurons, they next removed the ovaries from these mice.
Coss noted, “This allowed us to determine that these neurons in the brain, called gonadotropin-releasing hormone neurons, show changes in connectivity that affect how they function. The increased number of synapses cause them to be faster and have more pulses of hormone secretion.”
Her team also discovered that neurons “innervating” the ovaries—providing nerves to the ovaries—were more numerous in transgenic mice than in normal mice.
“We think the increases we see in ovarian hormone levels are due to increases in ovarian innervation rather than increases in hormone-producing cells. The endocrine perspective supports the latter,” Coss stated.
Next, Coss and her group want to find out if partly inhibiting neurons in the ovaries can lessen the consequences of the FMR1 mutation.
She concluded, “We anticipate this may normalize ovarian hormone levels, possibly allowing for a normal reproductive lifespan.”
Source:
Journal reference:
Villa, P. A., et al. (2023). Altered GnRH neuron and ovarian innervation characterize reproductive dysfunction linked to the Fragile X messenger ribonucleoprotein (Fmr1) gene mutation. Frontiers in Endocrinology. doi.org/10.3389/fendo.2023.1129534