Reviewed by Danielle Ellis, B.Sc.Aug 22 2023
A new study from the University of Minnesota is the first to show that gene therapy can mend neural connections in people with Hurler syndrome, a rare hereditary brain condition. The findings point to the adoption of gene therapy—an entirely new standard of treatment—for patients suffering from brain diseases like Hurler syndrome, which can be fatal.
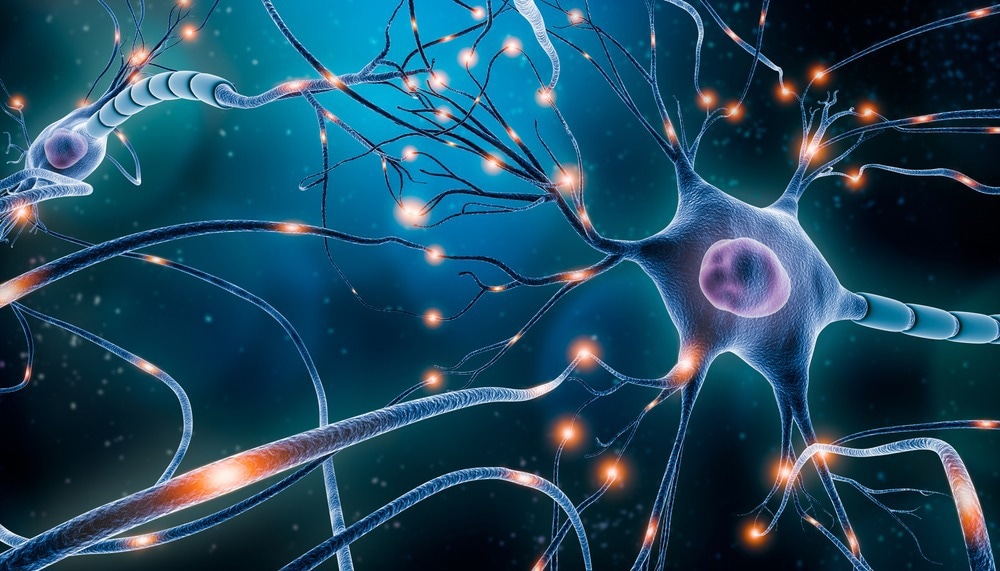
Image Credit: MattL_Images/Shutterstock.com
The findings were reported in the journal Nature journal Scientific Reports.
Hurler syndrome, commonly known as mucopolysaccharidosis type I (MPS I), is a genetic condition that affects neonates and causes significant cognitive and physical impairments. Mutations in the DNA of a critical lysosomal enzyme IDUA cause gradual brain injury.
Death happens before the age of ten. Current therapies are insufficient—bone marrow transplants are risky, and lifetime enzyme replacement is ineffective in preventing increasing brain deterioration.
The PS gene-editing technique, developed at the University of Minnesota, was tested in Hurler syndrome mice by the researchers. This method produced extremely high, constant levels of normal enzymes in the liver, which can reach the brain through the circulatory system.
Researchers initially detected damaged neural networks using high-resolution resting-state functional MRI (rs-fMRI), a safe, non-invasive, whole-brain activity imaging method for diagnosis and post-treatment evaluation. Following that, they analyzed the extent to which brain functions and connections were restored as a result of gene therapy.
The researchers discovered that the novel PS gene-editing method produced normal liver enzymes capable of maintaining normal connections within certain brain networks. Wei Zhu, a graduate student at the University’s Center for Magnetic Resonance Research, created the technology required for high-resolution rs-fMRI brain connectome imaging.
Walter Low, the study co-senior author, and professor at the University of Minnesota Medical School, called the study a milestone.
This is the first demonstration of a gene therapy that has corrected a neurological disorder resulting in the restoration of brain connectivity as confirmed by rs-fMRI.”
Walter Low, Study Co-Senior Author and Professor, University of Minnesota
Wei Chen, study co-senior author and professor in the U of M Medical School and Center for Magnetic Resonance Research, added, “A similar rs-fMRI approach as applied in this preclinical study should be translatable to the clinical setting and patients, especially for those with genetic brain disorders, and for examining the efficacy of brain network restoration and function after gene treatment.”
Chester Whitley, another study co-author and professor in the U of M Medical School, stated, “The aeonic production of normal IDUA in the liver of mice with Hurler syndrome and the ability to traffic enzymes across the blood-brain barrier to correct abnormalities in the brain is a significant achievement.”
“This new approach will enable the monitoring of brain connectivity in other lysosomal disorders that affect brain function following gene-editing,” Perry Hackett, study co-author and professor in the College of Biological Sciences, concluded.
Source:
Journal reference:
Zhu, W., et al. (2023). Mapping brain networks in MPS I mice and their restoration following gene therapy. Scientific Reports. doi.org/10.1038/s41598-023-39939-0