Reviewed by Danielle Ellis, B.Sc.Aug 22 2023
Investigators are learning more about how schizophrenia develops by investigating the most powerful known genetic risk factor. When a small portion of chromosome 3 is missing, a condition known as 3q29 deletion syndrome occurs, which increases the risk of schizophrenia by approximately 40-fold.
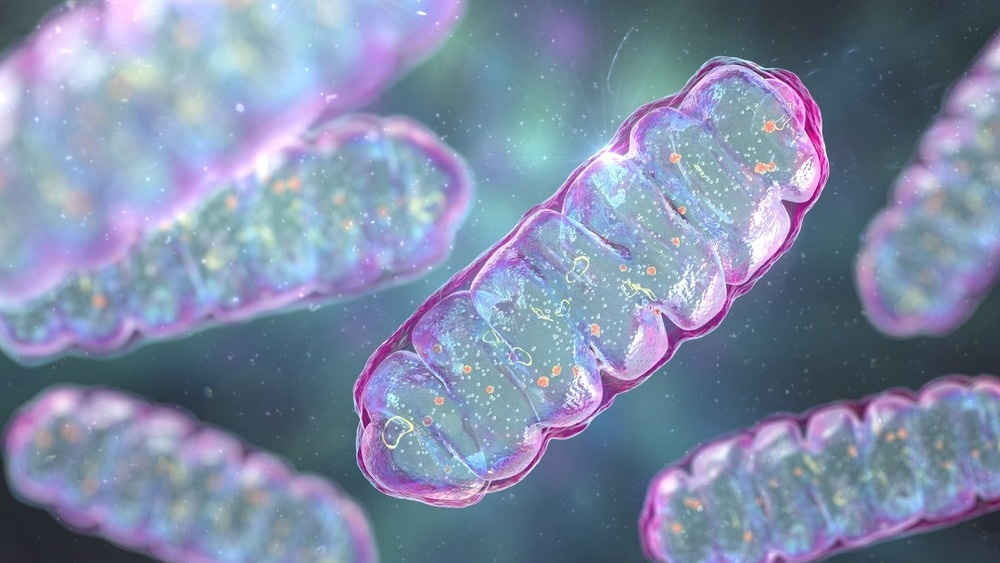
Image Credit: Kateryna Kon/Shutterstock.com
Researchers discovered an unexpected change in brain cells by analyzing how patterns of altered gene activity overlap in two models of 3q29 deletion syndrome—in mice and human brain organoids.
The findings are consistent with previous research on another genetic risk factor for schizophrenia, 22q11 deletion syndrome or DiGeorge syndrome, which has also been linked to impaired mitochondrial function.
The findings have been published in Science Advances.
For genetic variants associated with schizophrenia, we want to understand the primary pathology at the cellular level. This gives us a foothold, which may help cut through schizophrenia’s polygenic complexity and better understand the neurobiology.”
Ryan Purcell, PhD, Study Co-Lead Author and Assistant Professor, Cell Biology, Emory University School of Medicine
The study was the result of a collaboration between Emory and Rutgers researchers. The labs of co-senior author Gary Bassell PhD, Steven Sloan PhD, and Victor Faundez MD, PhD collaborated at Emory. Esra Sefik PhD, an Emory postdoctoral fellow who is now at Princeton, is the co-lead author.
Jennifer Mulle, PhD, and colleagues discovered that 3q29 deletion was a risk factor for schizophrenia in 2010. Mulle, who previously worked at Emory, is now an Associate Professor of Psychiatry, Neuroscience, and Cell Biology at Rutgers.
Our data give strong support to the hypothesis that mitochondrial dysregulation is a contributor to the development of schizophrenia. The interplay between mitochondrial dynamics and neuronal maturation is an important area for additional detailed and rigorous study.”
Jennifer Mulle, Associate Professor, Psychiatry, Neuroscience, and Cell Biology, Rutgers University
The prevalence of 3q29 deletion syndrome is estimated to be 1 in 30,000. 3q29 deletion can cause intellectual disability, autism spectrum disorder, and congenital heart defects, in addition to increasing the risk of schizophrenia. The effect of the 3q29 deletion on schizophrenia risk is greater than that of any single known gene variant, however, the contributions of individual genes within the deletion are still unknown.
The discovery that diverse schizophrenia-associated chromosomal deletions converge on mitochondria contradicts the field’s expectation that such mutations would affect proteins involved in synapses: the connections between neurons.
However, mitochondria are required for the function of energy-hungry synapses, so these models may not be in conflict. According to Bassell, more research is needed to determine whether mitochondria at synapses are particularly vulnerable.
It was also surprising to discover that 3q29 cells have dysregulated mitochondria because only one of the 22 genes in the deletion encodes a protein found in mitochondria. The 22q11 deletion, on the other hand, encompasses numerous genes encoding mitochondrial proteins. Purcell speculates that the 3q29 gene involved may indeed regulate the production or importation of mitochondrial proteins.
Mitochondria are found in every cell and use oxygen to generate energy in the form of ATP (adenosine triphosphate). Mitochondria have their own genomes, but the majority of the proteins found within them are encoded by genes in the nucleus of the cell.
3q29 cells lack metabolic flexibility as a result of modified mitochondrial function, making it difficult for them to adapt to changes in energy sources. This may disrupt neuronal development because maturing neurons must rely more on mitochondria for energy as they differentiate. Purcell is now testing whether cells from people with 22q11 have the same metabolic inflexibility, and is supported by a recently awarded grant.
Eventually, we want to understand which cellular changes like these are linked to specific clinical outcomes, which could help in designing more effective therapeutic strategies.”
Ryan Ryan Purcell PhD, Study Co-Lead Author and Assistant Professor, Cell Biology, Emory University School of Medicine
The findings show how the 3q29 deletion affects the entire body, not just the brain; the effects on mitochondria can be seen in kidney cells as well as brain cells. People with 3q29 deletion syndrome are also smaller than average, possibly due to altered fat metabolism.
Source:
Journal reference:
Purcell, R. H., et al. (2023) Cross-species analysis identifies mitochondrial dysregulation as a functional consequence of the schizophrenia-associated 3q29 deletion. Science Advances. doi.org/10.1126/sciadv.adh0558.