The University of Michigan Department of Neurosurgery and Rogel Cancer Center study demonstrates enticing early results that a therapy merging cell-killing and immune-stimulating drugs is effective and safe in prolonging survival for patients with gliomas, an extremely aggressive form of brain cancer.
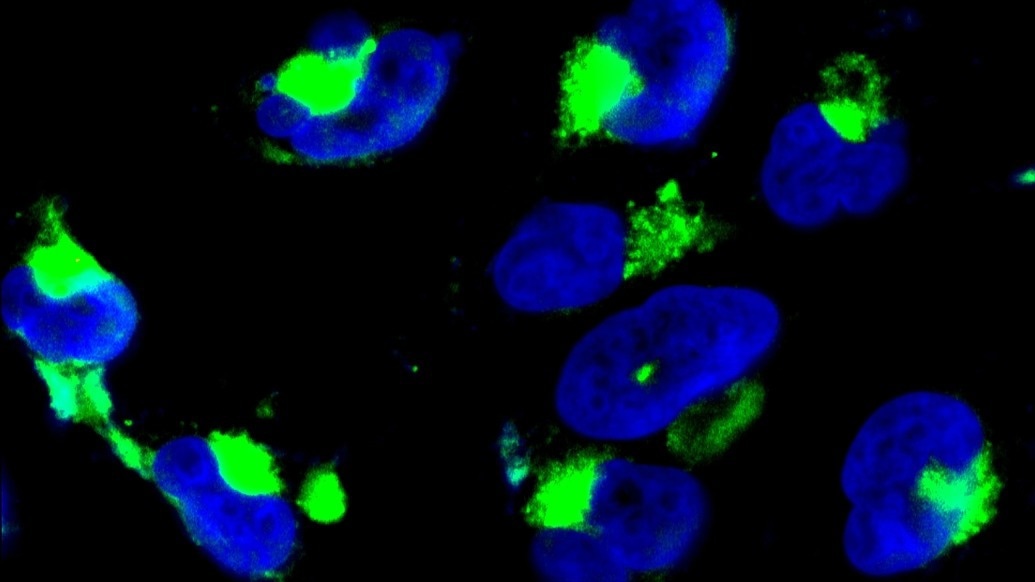
Image Credit: University of Michigan Department of Neurosurgery and Rogel Cancer Center.
The research was published in The Lancet Oncology.
Rogel researchers Pedro Lowenstein, MD, PhD, and Maria Castro, PhD, are the study’s lead authors. They earlier developed and investigated adenoviral-mediated gene therapies in their facility. This is a phase 1, first-in-human trial.
The team considered using the protein Flt3L to attract immune cells that are typically absent from the brain due to the poor prognosis of gliomas and their limited response to therapies like chemotherapy and radiation.
To start a more potent immune response against cancer, these immune cells are necessary.
Being able to move a novel therapy from bench to bedside in such a streamlined fashion is exciting, and represents a tour-de-force in translational medicine.”
Oren Sagher MD, Professor, Neurosurgery, University of Michigan
The research looked at two types of genetic therapies for high-grade gliomas.
The first was a combination of the protein HSV-1-TK and Valtrex, which is used to treat viral infections such as cold sores and chickenpox.
Valtrex is converted into a cytotoxic compound by HSV-1-TK, which kills actively dividing cancer cells. The second protein was Flt3L, which recruits important immune cells to the brain.
When used together, these therapies demonstrated promising early results, including increased survival. Six patients survived more than two years in the trial, three survived more than three years, and one patient, who is still alive at the time of publication, survived up to five years.
With prevailing standards of care, the life expectancy for this type of tumor is just over 14 months.
The study also discovered that this treatment was not toxic to the patients, implying that the highest dose used in this trial might be used in future trials.
Though the adenoviral gene therapy vectors were expected to be active for up to a month, researchers Maria Luisa Varela, PhD, Mohammad Faisal Syed, PhD, and Molly West, PhD found that activity from the adenoviral vector expressing the HSV1-TK could last up to 17 months.
This finding alters expectations for adenoviral gene therapy in the brain and broadens the time frame for which the combination of HSV1-TK and Valtrex could be used to combat tumor recurrence.
This originated from a theoretical idea based on evolutionary hypotheses and was first tested in experimental models of the disease.”
Pedro R Lowenstein, Richard C. Schneider Collegiate Professor, Neurosurgery, University of Michigan
“Finally, after many years, we’re thrilled to report the results of testing this approach in human patients, obtaining results that will lead to better treatments for this group of brain tumor patients,” notes Maria Castro, PhD, Rogel Member and Professor of Neurosurgery at U-M.
Although more research is needed before this can be used in the clinic, the importance of long-term expression of HSV1-TK suggests that it be implemented to improve treatment.
The findings support the design of future phase 1b/2 clinical trials.
Source:
Journal reference:
Umemura, Y., et al. (2023) Combined cytotoxic and immune-stimulatory gene therapy for primary adult high-grade glioma: a phase 1, first-in-human trial. The Lancet Oncology. doi.org/10.1016/S1470-2045(23)00347-9.