The thymus gland plays a vital role in both the endocrine and lymphatic systems and is responsible for the production and maturation of various types of immune cells. However, thymic function is extremely sensitive to infection and stress and also declines with age.
In a recent study published in Nature Immunology, a large team of scientists used advanced technologies such as spatial and single-cell transcriptomics, as well as lineage-tracing and imaging methods, to investigate the age-associated alterations in the thymus.
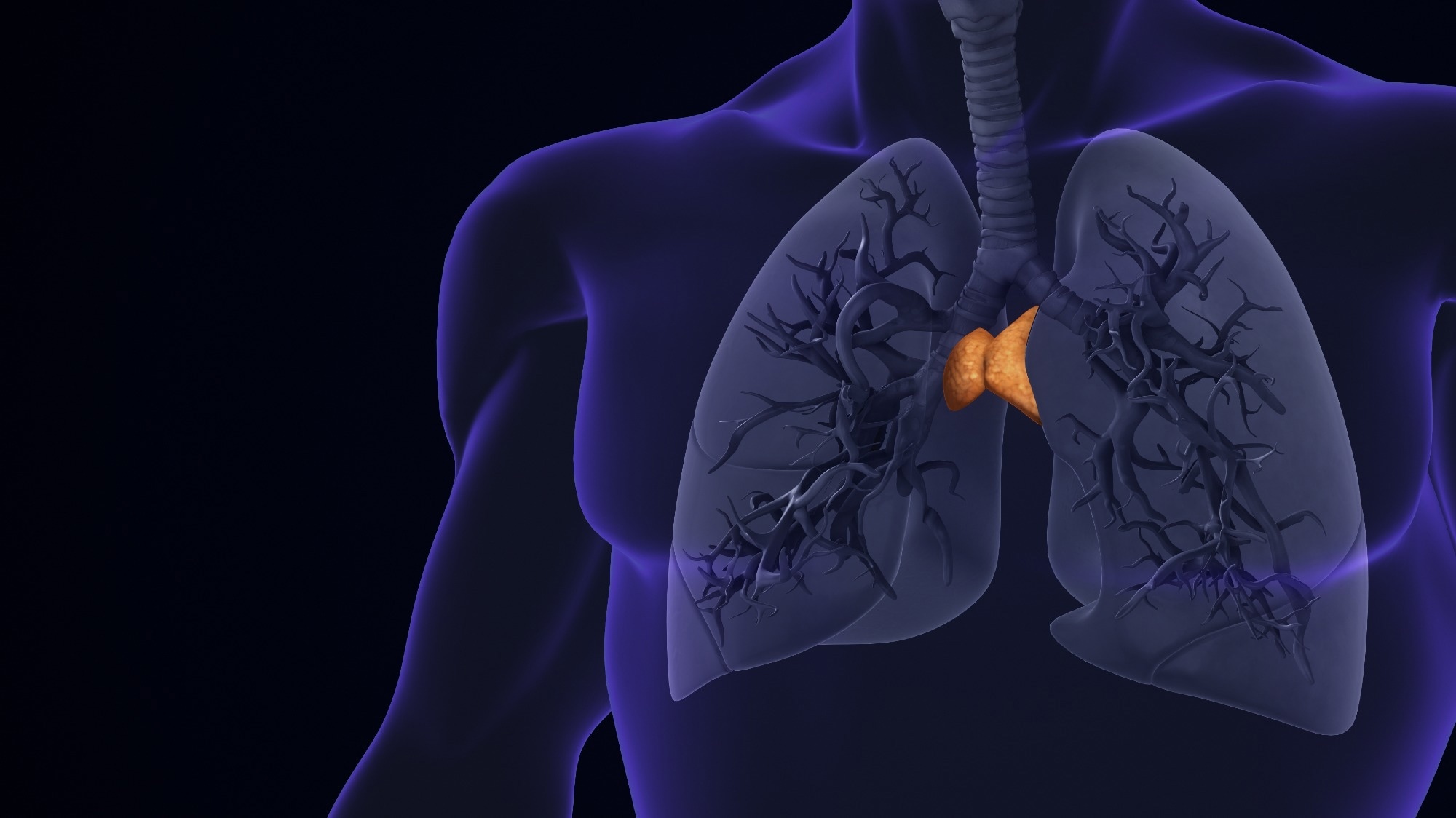 Study: Age-related epithelial defects limit thymic function and regeneration. Image Credit: Cinefootage Visuals/Shutterstock.com
Study: Age-related epithelial defects limit thymic function and regeneration. Image Credit: Cinefootage Visuals/Shutterstock.com
Background
The thymus gland is situated in the upper chest and is one of the major organs involved in the maturation of immune cells. The differentiation of T cells in the thymus is dependent on the interactions between the thymocytes and the cells surrounding the thymus, such as the endothelial cells and the thymic epithelial cells.
Although the thymus can regenerate, the thymic function undergoes significant age-related decline, with shrinkage of the thymic tissue, reduced T cell production, and various structural changes beginning immediately after puberty.
The organ is also sensitive to damage from infections and stress, as well as radiation and chemotherapy.
While it is known that this decrease in thymic function and the subsequent lowering of T cell counts leaves the body more vulnerable to infections and diseases, the underlying mechanisms behind the regeneration and age-related decline of the thymus are not well understood.
The Current Study
In the present study, the scientists used human tissue cultures and murine models and analyzed spatial and single-cell transcriptomics along with advanced imaging methods to investigate age and injury-related thymic loss of regeneration and decline in thymic function.
Injury to the thymus was modeled in the mice models using sublethal total body irradiation doses, after which the mice were euthanized, and the thymus glands were processed for tissue clearing and immunofluorescent staining using various antibodies.
Light-sheet and confocal microscopy were employed to visualize whole thymus lobes and tissue sections, respectively. These images were then used to analyze the volumes of the thymic regions and identify the subpopulations of thymic epithelial cells.
The researchers also obtained human thymus tissue samples, which were enzymatically digested and analyzed using cell sorting and flow cytometry to isolate the various types of cells.
Magnetic-activated cell sorting was used to enrich the samples for thymic epithelial cells. Various antibodies for intracellular and surface markers of different cell populations were also used during flow cytometry to isolate and identify the various cell types.
The isolated and sorted thymic cells were then analyzed using single-cell ribonucleic acid (RNA) sequencing (scRNAseq) and various computational analyses to understand their distributions and responses to injury.
The computational analyses included mapping the spatial and single-cell transcriptomes and an assessment of differentially expressed genes.
Additionally, a meta-analysis of the single-cell RNA data was also conducted, which included analysis of RNA velocity, cell fate prediction, pathway enrichment, cell-cell interactions, and networks.
Major Findings
The scientists discovered that with age, atypical epithelial cell clusters known as age-associated thymic epithelial cells (aaTECs) are formed in the thymus. These aaTECs lack thymocytes and contribute to the degeneration of thymic tissue. Furthermore, although age-related, the prevalence of aaTECs was also found to increase with injury.
The study identified the emergence of two aaTECs states that exhibit a partial transition from epithelial to mesenchymal state, along with down-regulation of the master transcription factor Foxn1 in the thymic epithelial cells.
The murine model experiments showed that injury exacerbated aaTEC accumulation in the thymus and reduced its capacity to regenerate.
Furthermore, the aaTECs also acted like a sink for regenerative signals, drawing these signals away from other thymic epithelial cells and contributing to decreased regeneration.
The scientists also believe that these structural alterations and changes in thymic function could be associated with molecular modifications in the thymic fibroblasts that could be linked to inflammaging, which is the chronic, low-grade inflammation that occurs with age.
Conclusions
To summarize, using single-cell RNA sequencing and spatial transcriptomics analysis, the researchers identified the emergence of two aaTEC states in the thymus due to age and injury.
The structural changes, such as decreased thymocyte levels and a transition from an epithelial to a mesenchymal state in aaTECs contribute to the decrease in the regenerative capacity of the thymus.
These findings are valuable for developing therapeutic strategies aimed at improving thymic function in aging adults.
Journal reference:
-
Kousa, A. I., Jahn, L., Zhao, K., Flores, A. E., Acenas, D., Lederer, E., Argyropoulos, K. V., Lemarquis, Andri L, Granadier, D., Cooper, K., D’Andrea, M., Sheridan, J. M., Tsai, J., Sikkema, L., Lazrak, A., Nichols, K., Lee, N., Ghale, R., Malard, F., & Andrlova, H. (2024). Age-related epithelial defects limit thymic function and regeneration. Nature Immunology. doi:10.1038/s41590024019159, https://www.nature.com/articles/s41590-024-01915-9