Diffuse midline gliomas (DMGs), characterized by H3K27M mutations, are highly aggressive pediatric brain cancers that mainly occur in young adults and children and have poor survival rates.
Standard treatments, such as radiotherapy and cytotoxic chemotherapy, have not been significantly beneficial, and immunotherapies and targeted therapies have provided limited benefit, highlighting the urgent need for novel therapeutic approaches.
In a recent study published in Nature, a team of scientists from Stanford University investigated the potential of chimeric antigen receptor (CAR) T-cell therapy specifically designed to target the disialoganglioside GD2, a molecule abundantly expressed in DMG cells.
The researchers evaluated the safety, feasibility, and preliminary efficacy of CAR T cell immunotherapy in treating DMGs through intravenous and intracerebroventricular administration.
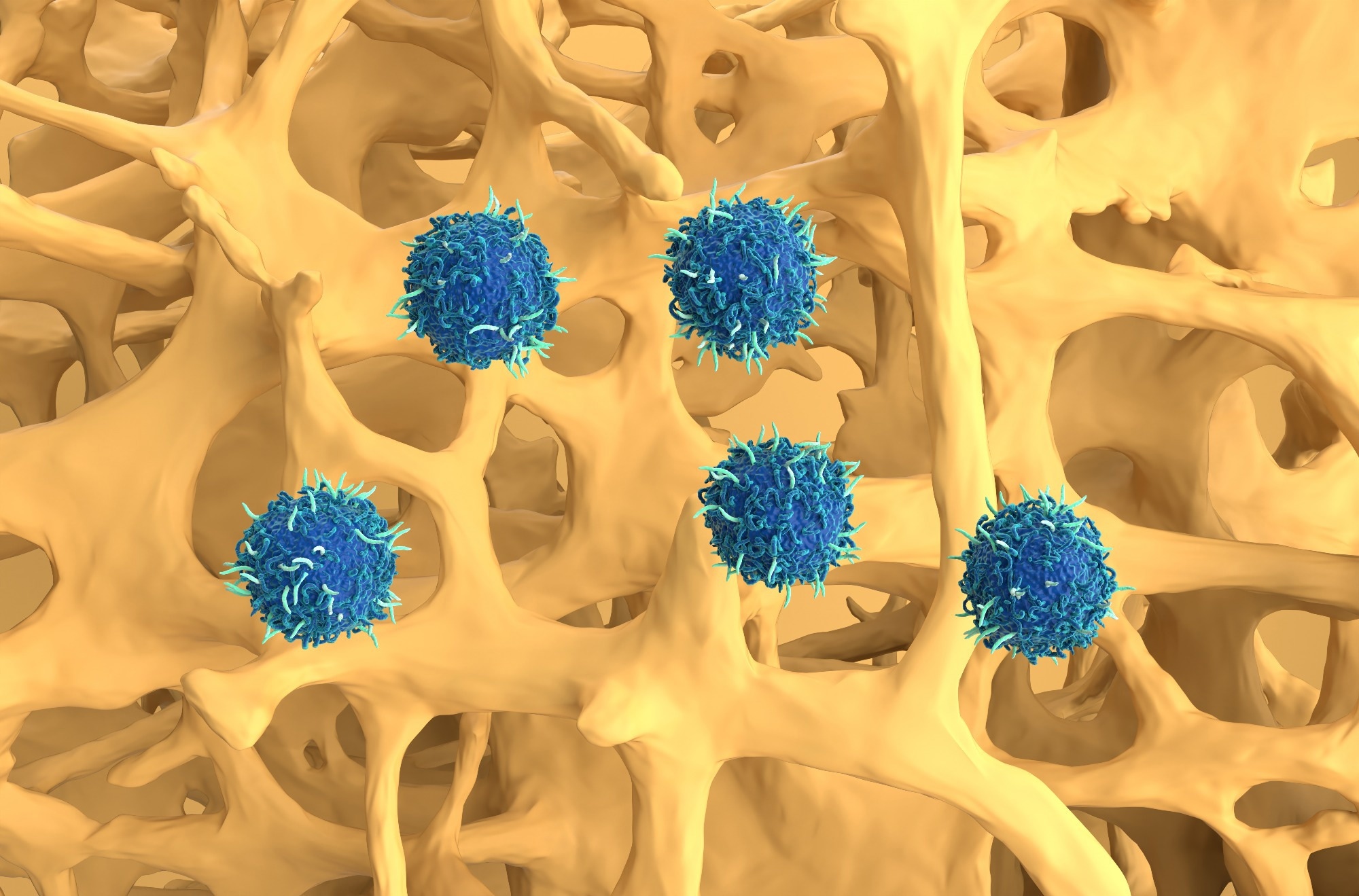 Study: Intravenous and intracranial GD2-CAR T cells for H3K27M+ diffuse midline gliomas. Image Credit: Nemes Laszlo/Shutterstock.com
Study: Intravenous and intracranial GD2-CAR T cells for H3K27M+ diffuse midline gliomas. Image Credit: Nemes Laszlo/Shutterstock.com
Background
Diffuse midline gliomas, including diffuse intrinsic pontine gliomas (DIPGs), are aggressive brain tumors primarily affecting children and the younger population.
Despite substantial advancements in oncology, the treatment options for DMGs remain limited, and survival outcomes are poor. The median survival for DIPG is approximately 11 months, and the long-term survival rates are under 1%.
While traditional therapies provide temporary symptom relief, they fail to significantly extend survival rates. Chemotherapy has shown little to no efficacy in improving outcomes. However, immunotherapy strategies have emerged as a promising avenue in cancer research, especially CAR T-cell therapies, which reprogram immune cells derived from the patient to target cancer-specific antigens.
Furthermore, recent studies have found that GD2 is uniformly expressed on DMG cells and could be a potentially viable target for CAR T-cell therapy, with preclinical research demonstrating the effectiveness of GD2-specific CAR T cells in eradicating tumor cells in experimental models.
About the Study
The present study was a phase I clinical trial to assess the efficacy, tolerability, and dosage of GD2-specific CAR T-cell therapy in patients aged 2 to 30 years with H3K27M-mutant DMGs who had completed standard radiotherapy.
The therapy involved two delivery methods — intravenous administration followed by intracerebroventricular infusions. The patients were divided into two dose levels for intravenous administration to determine the maximum tolerated dose. The eligibility criteria used in the study ensured that the participants had acceptable performance status and stable conditions post-radiotherapy to undergo this treatment.
GD2-specific CAR T cells were manufactured from patient-derived cells and genetically modified to target GD2. The researchers monitored the production process to ensure high viability and consistent CAR expression. Following the intravenous injections, eligible patients received intracerebroventricular infusions.
Lymphodepleting chemotherapy, which is a short course of chemotherapy that kills T cells in preparation for CAR T-cell therapy, preceded the intravenous administration but not the intracerebroventricular infusions, which were repeated once every one to three months based on clinical or imaging stability.
The researchers conducted rigorous safety protocols for monitoring for potential toxicities, such as cytokine release syndrome and neuroinflammation-related adverse effects. Additionally, advanced imaging and clinical assessments were used to evaluate tumor response and neurological improvement.
Furthermore, tumor volumetric analysis and clinical improvement scores were calculated to provide measures of therapeutic impact. At the same time, laboratory studies monitored CAR T-cell persistence, cytokine profiles, and tumor markers in blood and cerebrospinal fluid.
The study also explored strategies to mitigate neurotoxicity and optimize treatment delivery. This included using Ommaya catheters for intracranial pressure monitoring and administering supportive therapies for inflammation-related symptoms.
Major Findings
The study found that GD2-specific CAR T-cell therapy was a safe and promising potential option for treating H3K27M-mutant DMGs. Intravenous administration of GD2-specific CAR T-cell therapy at the lower dose level (DL1) was well-tolerated.
In contrast, the higher dose (DL2) led to cytokine release syndrome in three patients, indicating that DL1 was the maximum tolerated dose.
Furthermore, intracerebroventricular infusions, administered after intravenous therapy, caused no dose-limiting toxicities, establishing the safety and feasibility of GD2-specific CAR T-cell therapy.
Notably, tumor volumetric reductions were observed in several patients, with four showing significant decreases (52%–100%) and one achieving a complete response, which was sustained over 30 months.
Additionally, neurological benefits were noted in nine of the 11 treated patients, with improvements in motor functions, sensory deficits, and overall clinical condition.
While the imaging responses largely correlated with clinical improvements, the researchers noted that some patients showed neurological progress without substantial changes in tumor size.
Meanwhile, T-cell persistence and activity were evident in blood and cerebrospinal fluid, with sustained expansion and tumor-specific responses being observed after repeated intracerebroventricular infusions.
In addition, the biomarker analyses revealed signs of immune activation, such as elevated cytokines and reduced tumor-associated genetic markers in cerebrospinal fluid-linked therapeutic responses.
Additionally, the toxicity profiles highlighted manageable challenges, including cytokine release syndrome and tumor inflammation-associated neurotoxicity (TIAN).
Cytokine release syndrome was primarily associated with intravenous administration, while TIAN was more common after early intracerebroventricular infusions, but both were found to resolve with supportive care. No severe long-term adverse effects were linked to the therapy.
Conclusions
Overall, the study reported that GD2-specific CAR T-cell therapy resulted in tumor regression and clinical improvements in DMG patients, demonstrating its potential as a viable treatment for these aggressive cancers.
Furthermore, the results showed that the combination of intravenous and intracerebroventricular administration resulted in significant tumor reductions and neurological improvements in several patients.
While toxicity was manageable, the researchers believe that further research is needed to optimize dosing and administration routes.
These findings mark a significant step toward developing effective immunotherapies for high-risk brain tumors in pediatric and young adult populations.
Journal reference:
-
Monje, M., Mahdi, J., Majzner, R., Yeom, K. W., Schultz, L. M., Richards, R. M., Barsan, V., Song, K., Kamens, J., Baggott, C., Kunicki, M., Rietberg, Skyler P, Lim, A. S., Reschke, A., Mavroukakis, S., Egeler, E., Moon, J., Patel, S., Chinnasamy, H., & Erickson, C. (2024). Intravenous and intracranial GD2-CAR T cells for H3K27M+ diffuse midline gliomas. Nature. doi:10.1038/s41586024081719. https://www.nature.com/articles/s41586-024-08171-9