The blood-brain barrier (BBB) can be thought of as the interface between the brain and the rest of the vascular system and is a key player in Glioblastoma research.
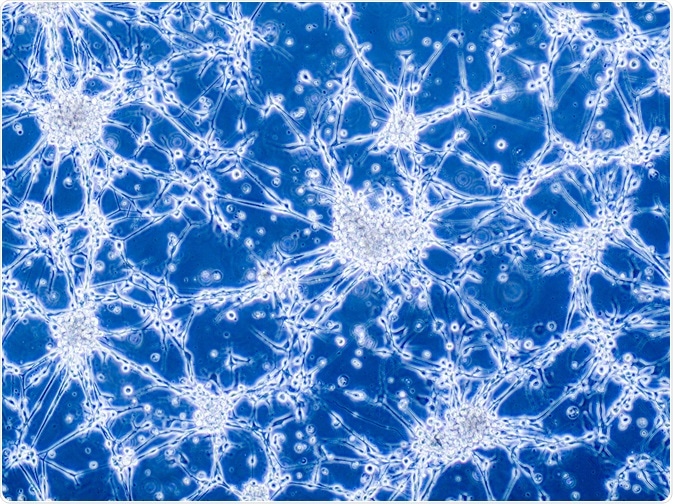
Image Credit: Anna Durinikova/Shutterstock.com
Metastasis, the development of secondary malignant growths, is the driving force behind brain tumors. The chances of brain metastasis will rise to 50% if other malignancies are found within the patient. This is because other cancer cells can successfully cross the BBB, and alterations of the BBB structure and function can lead to even an even greater progression of neurodegenerative diseases.
To harness a better understanding of the BBB, in vitro models with analogous structure and function are being made. Using mice as in vivo models is also performed when exploring the permeability of the BBB. These two approaches have and will continue to elucidate molecular mechanisms and novel therapeutic targeting agents.
What is the BBB?
The BBB is comprised of endothelial cells and controls the molecular flux between the blood and the nervous tissue. These cells line small capillaries to make up the matrix, packaged together tightly to make the intercellular space narrow. This is nature’s design, constructed this way to prevent toxins and foreign entities from entering the brain.
Though this helps prevent damage to the brain it also forms a hurdle, preventing drugs and medicinal moieties from passing the barrier. Unlike the dura and other facets of the meninges, the BBB is not leaky, preventing passage. Located in the brain capillaries, the BBB does not associate with arterials or venules, because the capillaries are the central site of exchange between the brain and blood.
Cerebral endothelial cell-based models have been developed to investigate brain metastasis through the BBB, in addition to the exploration of targeted anti-angiogenic medication. Though this has proven useful, a full-proof model for screening drugs for the brain has not yet been developed.
Contemporary labs have two distinct ways to screen for drugs and their passage through the BBB. One is through the use of animal models, a cornerstone of biomedical research. The other is to replicate a simplified 2D in vitro model of the BBB. Neither methodology is ideal.
In vivo murine models for BBB exploration
Most drug passage studies through in vivo BBB models incorporate smaller laboratory subjects, specifically mouse, rat, and other murine animals. According to their higher P- values of permeability coefficients, and higher reproducibility averages, these murine animals provide better surrogates for modeling. This mode of testing can yield elucidations on real-time transcytosis across the endothelial cell monolayer, and accurate measurements of the transendothelial electrical resistance (TEER).
TEER is the measurement of electrical resistance across the monolayer, and a vital component of the BBB. This is performed by measuring target concentrations in the blood and brain, followed by intramuscular injection and anesthetizing of the mouse itself-most commonly done through inhalation of isoflurane. The samples are immediately transferred into heparinized tubes where further tests can be done.
In vitro BBB models and their fabrication
In vitro 2D models are formed by co-culturing brain capillary endothelial cells, astrocytes, and pericytes. This provides an apropos model, and a platform to test drugs for brain disease. To assess the veracity of these varieties of BBB models, permeability and resistance measurements are taken.
The classic method of constructing the in vitro BBB is to extract microvessels from the target area and construct a model endothelium layer. It is also important to note that primary host endothelial cells would yield the most accurate depiction of the BBB, though this cannot always be accomplished.
To do this, grey matter is harvested, followed by enzymatic digestion and centrifugation. This is how microvessels can be isolated and analyzed via microscopy. After this stage, the centrifugated medium can bind to the extracellular matrix, and after subsequent washes, target microvessels can be segregated from the arterioles and venules.
Arterioles and venules are discounted to give a more apt model of the BBB. Though this washing will not eliminate these impurities, it does provide an apt model, yielding a quasi-pure culture of capillary endothelial cells.
Limitations of these methods
The limitation of using animal models is that the endothelial cells found in mice, rats, and other imitates are different from those in human physiology. The difference in exchange properties that are found across the animal kingdom contribute to the differences in endothelial cell properties.
The limitation of culturing the cells in this manner is the significant loss of brain matter that comes with digesting. When digesting this brain matter, collagen is also removed, which will release pericytes that grow faster than the endothelial cells themselves on account of their lesser complexity. This skewed cell ratio within the model will hinder the legitimacy of the model.
The limitations that pertain to in vitro models can sometimes be even greater than in vivo. Many of these single mono-layer endothelial cell lines only capture a fraction of the neurovascular network. This will hinder the physiological relevance of the model.
Sources:
- Molino, Y., Jabès, F., Lacassagne, E., Gaudin, N., & Khrestchatisky, M. (2014). Setting-up an in vitro model of rat blood-brain barrier (BBB): a focus on BBB impermeability and receptor-mediated transport. Journal of visualized experiments: JoVE, (88), e51278. https://doi.org/10.3791/51278
- Robin Augustine, Ahmad H. Aqel, Sumama Nuthana Kalva, K.S. Joshy, Ajisha Nayeem, Anwarul Hasan. (2021) Bioengineered microfluidic blood-brain barrier models in oncology research. Translational Oncology, Volume 14, Issue 7, 101087, ISSN 1936-5233
- Shayan G, Choi YS, Shusta EV, Shuler ML, Lee KH (2011). Murine in vitro model of the blood-brain barrier for evaluating drug transport. Eur J Pharm Sci.;42(1-2):148-55.
- Campos, S., Davey, P., Hird, A., Pressnail, B., Bilbao, J., Aviv, R. I., Symons, S., Pirouzmand, F., Sinclair, E., Culleton, S., Desa, E., Goh, P., & Chow, E. (2009). Brain metastasis from an unknown primary, or primary brain tumour? A diagnostic dilemma. Current oncology (Toronto, Ont.), 16(1), 62–66.
- Srinivasan, B., Kolli, A. R., Esch, M. B., Abaci, H. E., Shuler, M. L., & Hickman, J. J. (2015). TEER measurement techniques for in vitro barrier model systems. Journal of laboratory automation, 20(2), 107–126
- Tian, X., Brookes, O., & Battaglia, G. (2017). Pericytes from Mesenchymal Stem Cells as a model for the blood-brain barrier. Scientific reports, 7, 39676. https://doi.org/10.1038/srep39676
Further Reading