Cancer is known to have a high incidence rate as well as a high mortality rate on a global scale. The World Health Organization (WHO) has ascribed cancer as the first or second leading cause of death in 2019 for those before the age of 70 in 112 of 183 countries.
Image Credit: Kateryna Kon/Shutterstock.com
The disease burden for cancer in both incidence and mortality has been growing worldwide, which is reflective of an aging and growing population. GLOBOCAN 2020 has estimated the number of new cancer cases included 19.3 million, with 10 million deaths estimated globally in 2020.
Cancer can be an incurable disease in several patient cases, with the survival rate for more than five years differing for various types, including 98% for testicular cancer, 65% for cervical cancer, 90% for breast cancer, and 5% for pancreatic cancer.
Cancer Treatment
Traditionally, the treatment options for cancer comprise surgery, chemotherapy, and radiation therapy. Chemotherapy treatments provide toxicity to all cells, with these drugs impacting the rapidly dividing cells at a greater extent than healthy cells. However, this systemic approach still greatly impacts healthy cells, causing severe adverse effects such as the destruction of organs and even organ failure.
The limitations of conventional chemotherapy have led to a more targeted approach being explored, with targeted therapies directed towards specific biomarkers, including proteins, which result in the uncontrollable growth of cancerous cells.
Targeted agents comprise small molecules and inhibitors that inhibit various kinases, such as imatinib, targeted towards gene fusion and BCR-ABL, resulting in chronic myelogenous leukemia (CML).
Drug Sensitivity
While drugs can be developed to be more targeted to the type of cancer a patient has, it can still be challenging to predict how sensitive a patient’s cancer would be to that drug. It is possible that a patient does not respond to a drug treatment due to a lack of sensitivity, which results in further cancer growth and progression, even while a patient is receiving treatment.
To understand how a patient’s cancer may respond to drug treatment, it is possible to carry out an in vitro drug sensitivity and resistance test (DSRT). A DSRT test can be executed on cancerous cells or tissues sampled from a patient with a range of anti-cancer compounds being tested to define the sensitivity and resistance of a patient’s cancer.
This is significant as diseases are heterogeneous, and even with the same type of cancer, the underlying mutations may vary from patient to patient. Subsequently, this may translate to providing different treatment plans, accounting for resistance and specific pathophysiology.
DSRT can be used in combination with molecular or genomic profiling tests as the results can provide a comprehensive understanding of a patient’s cancer, enabling a more personalized approach to cancer treatment.
Additionally, the use of DSRT on cancer cells with a library of anti-cancer drug candidates as well as combinations can reveal which compounds result in sensitivity in the cancer sample and which compounds and combinations do not result in an effect. Interestingly, this type of testing can also reveal compounds that demonstrate sensitivity in the cancer cells that are not normally prescribed for a certain type of cancer – this is known as drug repurposing.
Repeating this test after a patient has received therapy can also be significant and useful as post-treatment cancer cells can help to detect resistant cells that were not destroyed after the first therapy. Using DSRT on these cells can be invaluable as it would consist of testing compounds and combinations that result in sensitivity in the cancer cell sample, which can then be prescribed as the second therapy to eliminate the resistant cell population.
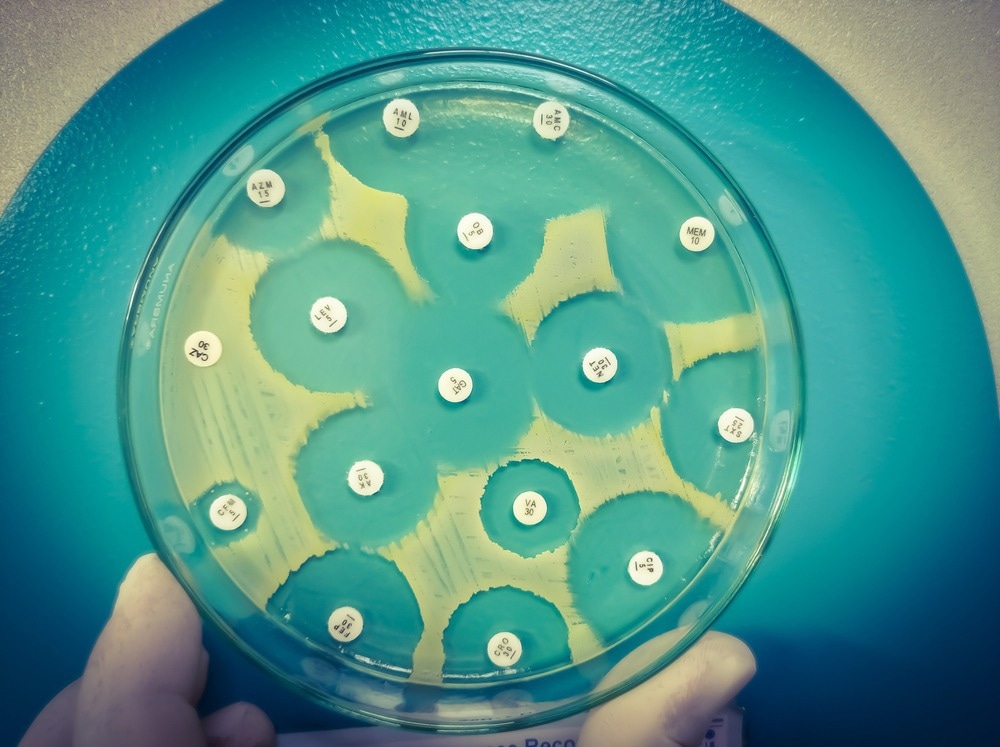
Image Credit: Babul Hosen/Shutterstock.com
DSRT using 2D and 3D cell models
The first DSRT of patient-derived cancer samples can be dated to the 1950s, with studies on in vitro tests on samples from patients with leukemia and solid tumors being published between the 1970s and 1990s.
DSRT on 2D cell culture models can be executed on cancer cells sampled from the blood or bone marrow of blood cancer patients or pieces of solid tumors once transitioned into a single cell suspension before testing.
This drug sensitivity test can vary in the predictability of clinical response, with published studies on DSRT using 2D and 3D cell models showing a range of results for different cancer types. DSRT using a 2D cell model of acute myeloid leukemia (AML), which consisted of 44 patients and ten different drug types, led to a 78% predictive response. Large studies and screening processes can consist of a drug panel of between 50 and 450 anti-cancer compounds.
DSRT testing on solid tumors can be more challenging than blood cancer samples due to having a limited number of cells within the sample as well as the preparation of solid tumors, which can be harsh in nature and further reduce the number of cells available. A further limited supply of cells for solid tumors can reduce the number of anti-cancer compounds tested on the cancerous cells and may include approximately 30 compounds.
Translational Significance
While the use of genomic and molecular profiling of patient cancers has become more common for personalized medicine, the combination of profiling and drug sensitivity tests can result in an overall beneficial and comprehensive understanding of a patient’s cancer.
Additionally, drug sensitivity and resistance tests take into account the heterogeneity of cancers, and the results of this test may reveal findings of an unusual anti-cancer compound that may have an unpredictably sensitive effect on cancer. This can guide oncologists on which anti-cancer compounds should be prescribed to patients and which compounds would be less likely to work.
This approach can help predict response rate, disease recurrence, drug resistance (including platinum-based drug resistance), and progression-free and overall survival in patients. Successful treatment management plans lead to more successful treatment and prognosis in patients, increasing their survival and quality of life – the most significant factor in healthcare.

 Read Next: Investigating the Role of Genomics in Cancer Detection
Read Next: Investigating the Role of Genomics in Cancer Detection
Sources:
- Lu, D.-Y. and Lu, T.-R. (2020) “Drug sensitivity testing, a unique drug selection strategy,” Advances in Biomarker Sciences and Technology, 2, pp. 59–66. Available at: https://doi.org/10.1016/j.abst.2020.11.001.
- Popova, A.A. and Levkin, P.A. (2020) “Precision medicine in oncology: In vitro drug sensitivity and resistance test (DSRT) for selection of personalized anti-cancer therapy,” Advanced Therapeutics, 3(2), p. 1900100. Available at: https://doi.org/10.1002/adtp.201900100.
- Sung, H. et al. (2021) “Global cancer statistics 2020: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries,” CA: A Cancer Journal for Clinicians, 71(3), pp. 209–249. Available at: https://doi.org/10.3322/caac.21660.
- Ulukaya, E., Karakas, D. and Dimas, K. (2021) “Tumor chemosensitivity assays are helpful for personalized cytotoxic treatments in cancer patients,” Medicina, 57(6), p. 636. Available at: https://doi.org/10.3390/medicina57060636.
Further Reading
Last Updated: Jan 30, 2023