The human leukocyte antigen (HLA) system plays an important role in maintaining the immunologic barrier against invading pathogens. Unfortunately, donor-specific HLA antibodies that develop as a result of organ/tissue transplantation, blood transfusions, pregnancies or other spontaneous can complicate various clinical scenarios.
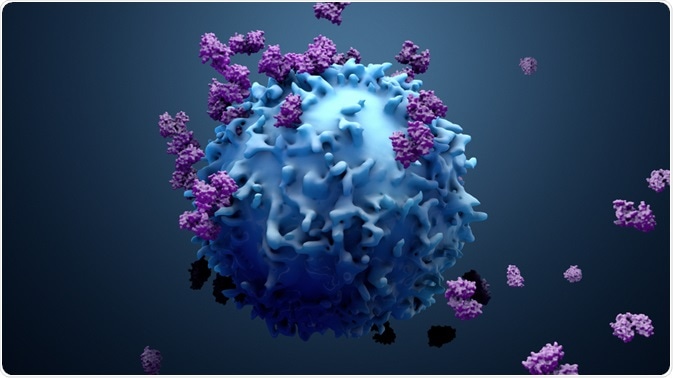
HLA. Image Credit: Design_Cells/Shutterstock.com
What are HLAs?
Originally discovered in the 1970s, Human Leukocyte Antigens (HLA) play a crucial role in how the immune system is capable of recognizing ‘self’ versus ‘non-self’ antigens. HLAs, which are often classified as major histocompatibility complexes (MHCs), can be further categorized as class Ia, which include HLA-a, HLA-B, and HLA-C, class Ib, of which include HLA-E, HLA-F, HLA-G, and HLA-H, as well as class II HLAs, of which include HLA-DR, HLA-DQ, HLA-DM, and HLA-DP. Class Ia and class Ib HLAs are responsible for presenting antigens to CD8+ cells and natural killer (NK) cells, respectively, whereas class II HLAs are involved in antigen presentation to CD4+ cells.
HLAs are associated with a high level of polymorphism, as they have several thousand alleles that are capable of encoding for functional polypeptides. This extreme polymorphism, coupled with its heterozygosity, allows the immune system to selectively target a diverse group of microorganisms and foreign antigens.
While these advantages allow HLAs to play a crucial role in the host’s immune response against pathogenic invaders, they also cause these proteins to be more susceptible to mutations and thus increases the risk of autoimmune diseases.
Risk factors for HLA sensitization
HLA antibodies can arise following exposure of the host immune system to non-self HLA molecules. HLA antibodies can develop spontaneously; however, some of the more common ways in which these antibodies can develop is during pregnancy, before or after the transplantation of foreign tissues, or following a blood transfusion.
Organ transplants
The organs that are more commonly implicated in HLA sensitization, both before and after the surgery, include the kidney, liver, heart, and lungs. Some of the different factors that can increase an individual’s risk of HLA sensitization include a prior tissue transplant, blood product infusion, pregnancy, or the use of a ventricular assist device. Of these risk factors, a history of a prior tissue transplant is considered to be the strongest.
Before any type of tissue transplant, transplant recipients will undergo histocompatibility testing to determine their immunologic risk to the tissue of the potential donor. This histocompatibility testing, which is also referred to as HLA typing, will provide information at the antigen or allele level of both the organ/tissue recipient and donor.
During HLA typing, an HLA mismatch can occur, which signifies that HLA antigens have been identified on the cells of the donor allograft but not in the recipient. A greater number of HLA mismatches will increase the “foreign appearance” of a donor tissue/organ to the recipient, thus increasing the risk that the recipient develops an alloimmune response.
Although the risk of HLA sensitization will increase in proportion to the number of HLA mismatches that have been identified during HLA typing, it is important to note that HLA sensitization can even occur with a zero mismatched graph.
Blood products
Although prior transplantation is considered to be the greatest risk of HLA sensitization, the sensitization risk that can result from the transfusion of various blood products is often underestimated. Despite the availability of erythropoiesis-stimulating agents (ESAs), pediatric patients with anemia, for example, are often vulnerable to developing blood requirements during acute illness.
Although there is a popular misconception that erythrocytes do not express HLA molecules, it has been shown that erythrocytes do express low levels of HLA class I molecules, The expression of HLA molecules is typically within the range of 100 to 2,000 per cell, which is comparable to the 10,000-20,000 HLA molecules that are present on leukocytes.
While this may be true, the large number of erythrocytes that are administered to patients during red cell transfusions significantly increases the risk of HLA sensitization.
In addition to the potential for sensitization that can occur following red cell transfusions, platelet products can also cause HLA sensitization. It is estimated that platelets contain a particularly high level of HLA molecules that is upwards of 81,000 molecules per platelet.
The storage of blood products can also potentially induce sensitization following transfusion as a result of the accumulation of leukocytes, white cell fragments, DNA, HLA peptides, cell debris, and pro-inflammatory cytokines.
Pregnancy
Non-classical HLA class Ib, which typically interacts with NK cells and other immune cells, plays an important role in maintaining an immunosuppressive state during pregnancy. By preserving maternal tolerance, HLA class Ib molecules, particularly HLA-G, contribute to fetal endurance and growth throughout the full gestation period.
In fact, a lack of HLA-G can have severe implications on the development of the fetus and result in spontaneous abortion and restricted fetal growth, as well as increase the mother’s risk of developing preeclampsia.
Spontaneous development
Some of the different environmental factors that have been proposed to be responsible for certain cases of spontaneous HLA sensitization include microorganisms, ingested proteins, and HLA allergens. In addition, certain pro-inflammatory events such as previous surgeries and/or trauma can also increase the patient’s risk of spontaneously developing HLA antibodies.
Spontaneous HLA antibodies are generally believed to be non-specific, which is comparable to those that develop following tissue/organ transplants, blood transfusions, and/or pregnancies.
Sources:
- Crux, N. B., & Elahi, S. (2017). Human Leukocyte Antigen (HLA) and Immune Regulation: How Do Classical and Non-Classicla HLA Alleles Modulate Immune Response to Human Immunodeficiency Virus and Hepatitis C Virus Infections? Frontiers in Immunology. doi:10.3389/fimmu.2017.00832.
- Rees, L., & Kim, J. J. (2015). HLA sensitization: can in be prevented? Pediatric Nephrology 30(4); 577-587. doi:10.1007/s00467-014-2868-6.
- Abbes, S., Metjian, A., Gray, A., et al. (2017). HLA sensitization in solid organ transplantation: a primer on terminology, testing, and clinical significance for the apheresis practitioner. Therapeutic Apheresis and Dialysis 21(5); 441-450. doi:10.1111/1744-9987.12570.
- Singh, M., Rajak, J., Kadam, S., & Rajadhyaksha, S. B. (2019). Alloimmunization and the Role of HLA in Pregnancy. Complications of Pregnancy. doi:10.5772/intechopen.84211.
Further Reading