Precision medicine is capable of customizing treatments according to the unique genetic sequence of a patient. However, to achieve this precision, or to develop novel drugs, it is important to know the types of genes involved in the disease.
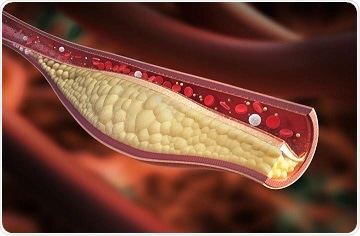
Work by Brian Parks and collaborators provides a new target for understanding the genetic risk of high cholesterol, which is linked to heart disease. Image Credit: Centers for Disease Control and Prevention.
Unfortunately, we don’t really have a good understanding of how these genetic differences can derive differences in traits, whether that’s cholesterol or obesity.”
Brian Parks, Professor of Nutritional Sciences, University of Wisconsin–Madison
Hence, to resolve these restrictions, Parks and his colleagues have developed a novel technique that can pick formerly unidentified genes out of the dark.
The scientists eventually identified a novel gene that regulates the body’s cholesterol by integrating the fine-grained detail available from animal research with the statistical power of genetic research involving scores of human genomes.
The study offers a novel target for interpreting the genetic risk of high cholesterol, which has been associated with heart disease. More significantly, the study offers a new method to expose how genetic changes can lead to several human diseases, which is the initial step toward treating them.
Parks and his team members from other universities have recently published the results of their study in the Cell Metabolism journal. The newly discovered gene called Sestrin1 controls the levels of cholesterol by blocking its production in the liver when a sufficient amount of the essential nutrient is provided by food.
The relative strengths of human and animal studies were integral to the team’s findings. Parks’ research team could employ mouse livers to analyze the genetic networks that contribute to cholesterol production, offering data that is seldom available in humans.
The researchers discovered as many as 112 genes that are associated with known cholesterol genetic networks.
The scientists then observed these 112 genes to find out which of these genes overlapped with possible cholesterol-linked DNA sequences in humans.
The human data was obtained from vast genetic studies that build up health data in an attempt to identify a connection between the disease and genes.
We can do these very large studies in humans of 500,000 people, and we can identify regions of the genome that are associated with, say, differences in blood cholesterol, But that just gives us kind of a lamppost to shine a light. It doesn’t tell us what underlying gene or pathway is potentially contributing to that association.”
Brian Parks, Professor of Nutritional Sciences, University of Wisconsin–Madison
Among the 112 genes that were initially started by the researchers, 54 were associated with the human data.
And most of them are well-known to be involved in cholesterol or liquid metabolism. But we were interested in the ones that were unknown.”
Brian Parks, Professor of Nutritional Sciences, University of Wisconsin–Madison
Of those genes, 25 had not been previously associated with humans’ cholesterol levels, making them promising new targets. Parks’ research team analyzed all the 25 genes in mouse models and evaluated them against fresh sets of human genomic data. The Sestrin1 gene stood out.
While the Sestrin1gene had never been linked with cholesterol before, the researchers discovered that it helps control the blood’s cholesterol levels. It supports the production of cholesterol until it is blocked by the diet’s cholesterol.
Mice lacking the gene were not able to control their cholesterol levels correctly. As a result, they developed high cholesterol while ingesting foods containing normal cholesterol levels because their livers did not respond correctly.
The scientists added that they had the benefit of studying cholesterol, which is mainly regulated by only a single tissue, the liver. However, the researchers’ technique of integrating human and mouse data has the potential to help expose other formerly unidentified genes, an immense support for interpreting and treating diseases.
“The possibility certainly exists to extend this technique to other traits like obesity,” Parks concluded.
Source:
Journal reference:
Li, Z., et al. (2020) Integrating Mouse and Human Genetic Data to Move beyond GWAS and Identify Causal Genes in Cholesterol Metabolism. Cell Metabolism. doi.org/10.1016/j.cmet.2020.02.015.