A team of researchers from the University of Toronto has plotted the genes that enable cancer cells to avoid being destroyed by the immune system—a discovery that could lead to the development of new immunotherapies that would be effective for larger populations of patients and across different types of tumors.
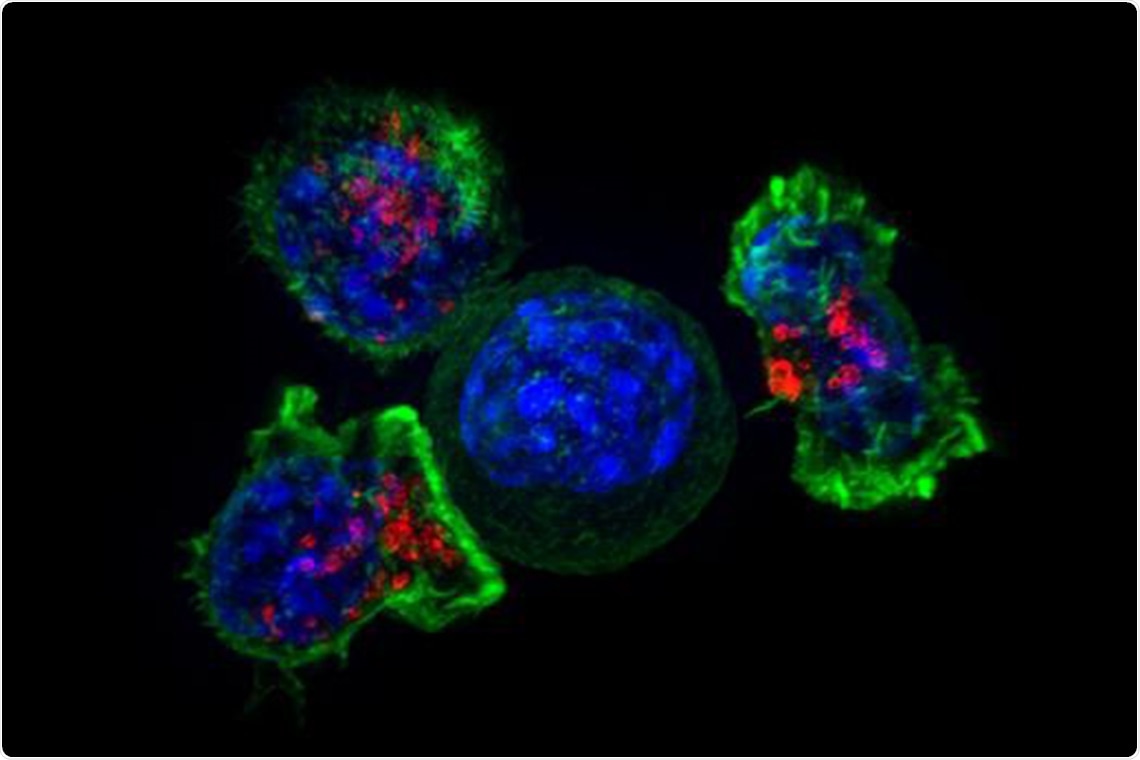
A cancer cell is surrounded by immune T killer cells. Image Credit: National Institutes of Health.
Over the last decade, different forms of immunotherapy have emerged as really potent cancer treatments, but the reality is that they only generate durable responses in a fraction of patients and not for all tumour types.”
Jason Moffat, Study Lead and Professor of Molecular Genetics, Donnelly Centre for Cellular and Biomolecular Research, University of Toronto
Published in the Nature journal, the study also demonstrated the need for novel therapy to consider the genetic composition of tumors owing to mutations in cancer cells. Such mutations, often known as “cancer resistance mutations,” can possibly make the disease worse in response to treatment.
According to Moffat, who holds Canada Research Chair in Functional Genomics of Cancer, “It’s very important to understand at the molecular level how cancer develops resistance to immunotherapies in order to make them more broadly available. Advances in systematic genetic approaches have let us key in on genes and molecular pathways that are commonly involved in resistance to therapy.”
In immunotherapy, a person’s own immune cells, called T killer cells are designed to identify and kill cancer. However, treatment resistance has prevented its use in a majority of the patients, particularly those with solid tumors.
It’s an ongoing battle between the immune system and cancer, where the immune system is trying to find and kill the cancer whereas the cancer’s job is to evade that killing.”
Keith Lawson, Study Co-Lead Author, Faculty of Medicine, University of Toronto
Keith Lawson will shortly complete a PhD in Moffat’s laboratory as part of his medical training in the surgeon-scientist program at Faculty of Medicine in the University of Toronto.
Tumor heterogeneity—that is, genetic changes in tumor cells within and across people that can influence therapy response—also complicates things.
Lawson added, “It’s important to not just find genes that can regulate immune evasion in one model of cancer, but what you really want are to find those genes that you can manipulate in cancer cells across many models because those are going to make the best therapeutic targets.”
The researchers, which included colleagues from Agios Pharmaceuticals in Cambridge, Massachusetts, prepared for genes that control immune evasion over six genetically diverse tumor models acquired from colon, breast, skin, and kidney cancer.
The cancer cells were located in a dish alongside the T cells designed to destroy them, where the resulting onslaught acted as a baseline. Later, the team posted CRISPR—the gene editing tool—to turn off every gene in the cancer cells gradually and quantified the resulting deviations from the killing baseline.
The team detected a total of 182 “core cancer intrinsic immune evasion genes,” whose deletion renders the cancer cells either more resistant or more sensitive to T cell attack. Among these resisters were all the genes believed to develop mutations in patients who no longer responded to immunotherapy. This provided confidence to the team that their method actually worked.
Several of the identified genes had no prior connections to immune evasion.
Lawson added, “That was really exciting to see, because it means that our dataset was very rich in new biological information.”
Genes that play a role in autophagy—a biological process when cells ramp up recycling their components to reduce damage subsequent to stress—was identified to be a key for immune evasion. This increases the chance that cancer’s sensitivity to immunotherapy could be improved by targeting its autophagy genes.
However as the researchers explored deeper, they identified that deleting specific autophagy genes in pairs made the cells resistant against T cell killing. This implies that if a tumor already has a mutation in one autophagy gene, a therapy that integrates immunotherapy with a medication targeting another autophagy gene could make the disease worse in that specific patient.
We found this complete inversion of gene dependency. We did not anticipate this at all. What it shows us is that genetic context—what mutations are present—very much dictates whether the introduction of the second mutation will cause no effect, resistance or sensitivity to therapy.”
Jason Moffat, Professor of Molecular Genetics, Donnelly Centre for Cellular and Biomolecular Research, University of Toronto
As more studies investigate the combinatorial effects of mutations across diverse types of cancer cells, it should probably become feasible to estimate from a tumor’s DNA of the type of therapy that will be most effective.
Source:
Journal reference:
Lawson, K. A., et al. (2020) Functional genomic landscape of cancer-intrinsic evasion of killing by T cells. Nature. doi.org/10.1038/s41586-020-2746-2.