Researchers from the University of Exeter have discovered a new method to “rescue” genetically mutated cells, providing more opportunities to develop a promising, new treatment for mitochondrial disease and other similar rare terminal childhood diseases.
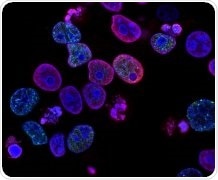
The team used novel drugs being developed at the University of Exeter, which “metabolically reprogramme” mitochondria. Image Credit: University of Exeter.
Financially supported by the United Mitochondrial Disease Foundation in the United States, the study was headed by Professors Matt Whiteman and Tim Etheridge. In the latest study, the researchers used novel medications that are being designed at the University of Exeter, which “metabolically reprogram” the cellular energy production centers in cells called mitochondria, by supplying them with an alternative source of fuel to produce metabolic energy in the form of small amounts of hydrogen sulfide.
The study was published in the Journal of Inherited Metabolic Disease.
The researchers used tiny worms (C. elegans) with particular genetic mutations influencing energy production, that match the mutations responsible for causing human diseases, like Leigh Syndrome.
The researchers observed that when the new compounds were injected into these worms, these compounds effectively enhanced or normalized energy production required to maintain the animals in healthy and active states.
Worms are a very powerful genetic tool to study human health and disease and offer an ideal platform to quickly identify new potential therapeutics. The worms used in this study had genetic defects in how their mitochondria regulate cellular energy production to model different human mitochondrial diseases.”
Tim Etheridge, Study Author and Professor, University of Exeter
Professor Etheridge continued, “The novel compounds we are developing at the University of Exeter are able to bypass some of these defects and keep the worms, and their mitochondria healthy. We know this because we saw improvements in physical activity and improvements in muscle and mitochondrial integrity. The animals also lived for longer after treatment but more importantly, they remained active for longer, because of metabolic reprogramming.”
Earlier, the researchers had demonstrated that the compounds had strong therapeutic effects in mammalian models with impaired mitochondria. In such studies, the mitochondria of the animals became defective because of a disease process.
But in the recent study, the impaired mitochondria were directly responsible for causing the disease, as in human mitochondrial disease, and were still effectively treated with the compounds developed by the University of Exeter.
The fact that the new compounds may reverse certain inherited defects in energy metabolism clearly indicates that their impact will translate to human beings, and the researchers are optimistic that this can be validated in the near future.
Mitochondrial diseases, and their related conditions, are areas of huge and desperate unmet clinical need. Our study is an important first step and a lot of work still needs to be done. For the first time, we have demonstrated that our new molecules have successfully metabolically reprogrammed, or rescued, cells in animals with genetic defects in their mitochondria.”
Matt Whiteman, Study Lead Author and Professor, University of Exeter
“We’re currently testing newer and more potent molecules able to do the same task, through slightly different approaches, and we’re looking for commercial partners to help our efforts to progress our molecules through to clinical testing,” Professor Whiteman concluded.
Source:
Journal reference:
Fox, B. C., et al. (2020) The Mitochondria‐Targeted Hydrogen Sulfide Donor AP39 Improves Health and Mitochondrial Function in a C. Elegans Primary Mitochondrial Disease Model. Journal of Inherited Metabolic Disease. doi.org/10.1002/jimd.12345.