Hepatitis C virus (HCV) can cause chronic liver infection, which can lead to irreparable liver damage and liver cancer. It is unclear how HCV manages to avoid the immune system and infect the host on a long-term basis.
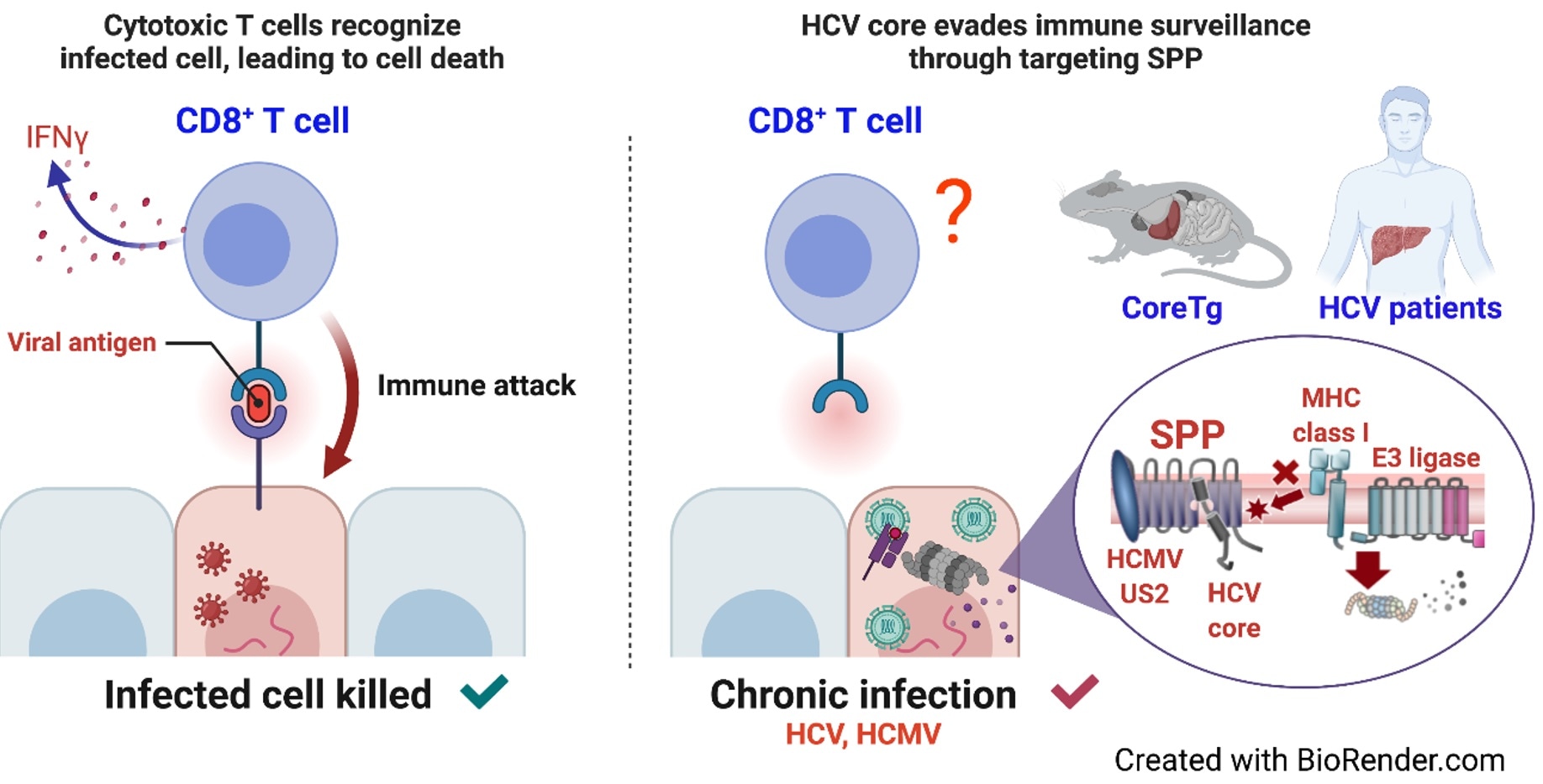
The researchers demonstrated how HCV and HCMV evade antigen presentation on MHC class I molecules. Expression of the HCV core protein or HCMV U2 protein inhibited SPP and subsequently induced degradation of MHC class I molecules. The researchers also discovered an impairment of MHC class I molecules in CoreTg mice and patients infected with HCV. We found that the HCV core protein interfered with the interaction of SPP with HLA-A, thereby inducing the accumulation of immature HLAs and subsequent HRD1-dependent degradation by proteasomes. Image Credit: Osaka University.
Osaka University researchers found a unique molecular mechanism through which HCV interacts with the host’s immune system to produce chronic liver infection in a recent study. These results might pave the way for the development of a novel treatment for chronic HCV infection.
In around 80% of individuals, HCV infection progresses to chronicity. Although antiviral therapies exist and can improve patients’ circumstances, they are insufficient in preventing liver damage and, as a result, the development of liver cancer.
To assist researchers and to create newer and improved therapies against the illness, it is critical to understand how HCV manages to avoid the host’s immune system in the first place, allowing it to become chronically settled.
HCV creates a single protein in infected cells, which is subsequently broken into 10 separate proteins at the molecular level. One of these proteins is the HCV core protein, which needs the action of a host cell protein, signal peptide peptidase (SPP), to function properly.
Researchers know that inhibiting SPP causes the HCV core protein to be broken down, which reduces the production of infectious HCV particles. However, until today, the mechanisms by which the core protein influences the host’s immune system were unknown.
Immunoevasins, which are proteins that help viruses evade the host’s immune system, exist in a number of viruses, such as Epstein–Barr virus, ebolavirus, cytomegalovirus, and hepatitis C virus. When cells are infected with a virus, they degrade viral proteins and load the fragments onto so-called MHC class I proteins, so that specific immune cells can sense the ongoing viral infection from outside the infected cells and eliminate them.”
Junki Hirano, Study First Author, Osaka University
“In this study, we wanted to understand the connection between signal peptide peptidase and MHC class I proteins in the setting of hepatitis C infection,” added Hirano.
To accomplish their aim, the researchers initially used a human liver cell line to study the interactions of the HCV core protein, SPP, and MHC class I proteins. They discovered that SPP is essential for the synthesis of MHC class I molecules in liver cells to have a proper immunological response.
In the presence of the HCV core protein, however, SPP is unable to adequately bind with MHC class I proteins, which are then destroyed by the activities of another protein, HMG-CoA reductase degradation 1 homolog (HRD1). As a result, the cellular presentation of virus particles to immune cells is hindered, and the infection becomes chronic.
The researchers then wondered if this was a typical technique used by other viruses to evade the host’s immune system. They resorted to human cytomegalovirus (HCMV), a virus known to harm the liver as well as other organs including the eyes and the esophagus.
They discovered that the US2 protein, which is generated by HCMV, is structurally identical to the HCV core protein and, similarly, causes the destruction of MHC class I proteins by targeting SPP.
These are striking results that show how HCV and HCMV may cause chronic infection by targeting signal peptide peptidase to achieve immune evasion. Our study revealed a novel molecular mechanism by which these viruses target an important component of the human immune system, MHC class I molecules, to interfere with the proper immune response. These findings could help with development of novel therapies against persistent infection caused by these viruses.”
Toru Okamoto, Study Lead Author and Professor, Osaka University