Reviewed by Danielle Ellis, B.Sc.Sep 14 2022
The human immune system is notably adept at evading tumor cells, which construct physical barriers, adopt masks, and restrain the immune system with molecular ploys. To overcome some of these obstacles and label cancer cells for immune system eradication, UC San Francisco researchers have now created a drug.
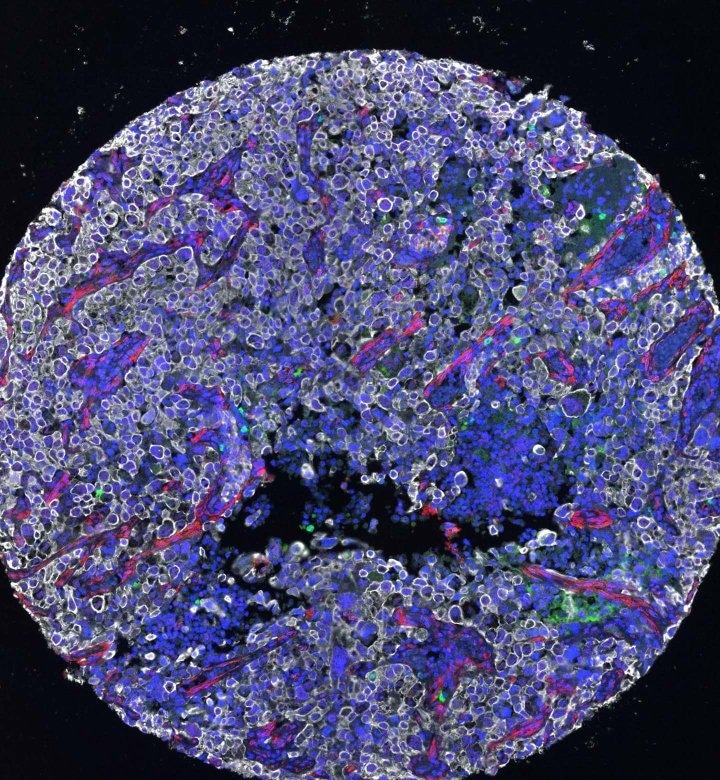 Microscopy of a lung tumor biopsy. Image Credit: Lin Ma
Microscopy of a lung tumor biopsy. Image Credit: Lin Ma
A mutant form of the protein KRAS is attracted to the surface of cancer cells by the new medicine, which works as a “eat me” flag when combined with the medicine. The immune system can then be stimulated by immunotherapy to successfully destroy all cells displaying this flag.
The immune system already has the potential to recognize mutated KRAS, but it usually can’t find it very well. When we put this marker on the protein, it becomes much easier for the immune system.”
Kevan Shokat, Howard Hughes Medical Institute Investigator and Chemist, University of California San Francisco
KRAS mutations are one of the most prevalent gene mutations in cancer, present in roughly 25% of tumors. Sotorasib, which the Food and Drug Administration (FDA) has granted provisional approval for use in treating lung cancer, also targets mutated KRAS, and it is possible that the two treatments could eventually function well together.
It is exciting to have a new strategy leveraging the immune system that we can combine with targeted KRAS drugs. We suspect that this could lead to deeper and longer responses for cancer patients.”
Charles Craik, Study Lead Author and Professor, Pharmaceutical Chemistry, University of California San Francisco
Turning cancer markers inside out
Foreign cells are frequently identified by the immune system due to the peculiar proteins that protrude from their surfaces. However, there are not many distinctive proteins on the exterior of cancer cells. Instead, the majority of the proteins that distinguish tumor cells from normal cells are found inside the cells, out of reach of the immune system.
Despite the fact that KRAS is frequently found in tumors, it was long thought to be insurmountable. The altered KRAS protein functions inside cells to promote the development of tumor cells. It frequently only varies from regular KRAS by a single minor mutation, and it lacks an obvious place on its structure where a drug could bind.
Shokat, however, has conducted thorough investigations of the protein in recent years and found a potent and selective area in mutant KRAS. His work aided in the creation and endorsement of sotorasib.
However, not all patients with KRAS mutations benefit from sotorasib, and some cancers that do shrink eventually develop resistance and recur. If there was another way to target KRAS, Shokat, Craik, and their colleagues challenged it.
The team's latest research demonstrates that ARS1620, a targeted KRAS drug similar to sotorasib, binds to mutant KRAS and does more than simply prevent KRAS from influencing tumor growth. Additionally, it induces the cell to identify the ARS1620-KRAS complex as a foreign substance.
“This mutated protein is usually flying under the radar because it is so similar to the healthy protein. But when you attach this drug to it, it gets spotted right away,” Craik added.
This indicates that the protein is processed by the cell and moved to its surface as a warning to the immune system. The KRAS that was once concealed within is now visible on the exterior of the tumor cells like a “eat me” flag.
A promising immunotherapy
The UCSF team was then able to scan a database of billions of human antibodies to locate those that could now recognize this KRAS flag as the mutant KRAS had migrated from the inside to the exterior of cells.
The most promising antibody they had found could bind strongly to both the drug ARS1620 and the ARS1620-KRAS complex, the researchers demonstrated in testing on both isolated protein and human cells.
The team then developed immunotherapy centered on that antibody, encouraging the immune system’s T cells to detect the KRAS flag and select cells for elimination. They discovered that tumor cells treated with ARS1620 that had mutated KRAS could be destroyed by the new immunotherapy, even if they had previously established resistance to the drug.
Shokat added, “What we have shown here is proof of principle that a cell resistant to current drugs can be killed by our strategy.”
Prior to the treatment being used in clinical settings, more studies are required both in humans and animals. According to the researchers, the new approach could pave the path for other similar combinations of targeted drugs and immunotherapies as well as combination therapy for cancers with KRAS mutations.
Craik further stated, “This is a platform technology. We would like to go after other targets that might also move molecules to the cell surface and make them amenable to immunotherapy.”
Source:
Journal reference:
Zhang, Z., et al (2022) A covalent inhibitor of K-Ras(G12C) induces MHC class I presentation of haptenated peptide neoepitopes targetable by immunotherapy. Cancer Cell. doi:10.1016/j.ccell.2022.07.005