The human immune system is expected to guard people against the invasion of external microbes, but at times, it turns its efforts inward, possibly leading to autoimmune disorders.
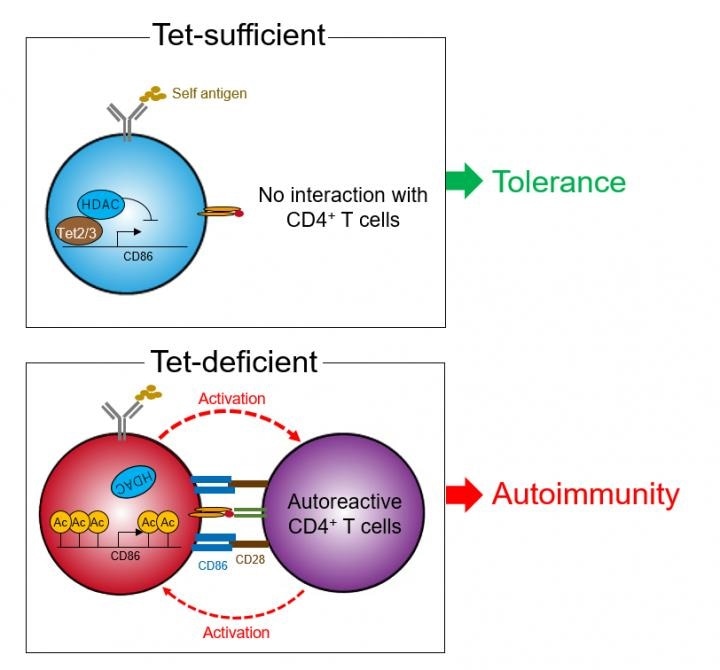
Tet2/3-deficient B cells are activated by self-antigen and express an exaggerated amount of CD86. Then those B cells stimulate autoreactive CD4+ T cells, resulting in autoimmune response. Image Credit: Osaka University.
In a recent study, Osaka University scientists found how reversible changes to human DNA by specific proteins guard individuals from autoimmune disorders and, on the other hand, how the lack of these proteins opens the door to autoimmunity.
All information is present in DNA. Cells in the human body need this information to function by offering specific codes to generate specific proteins. However, it is not always possible to access the entire parts of the DNA in all the cells.
The controlled synthesis of proteins ensures that different organs and cells can be developed from the same type of DNA code. A significant regulatory mechanism is a reversible removal (demethylation) and addition (methylation) of chemical bonds—the supposed methyl groups—to DNA segments. The readout of the said DNA segment is altered by this mechanism.
Proteins of the ten-eleven translocation (Tet) family are familiar with DNA demethylases that reduce the generation of specific proteins in immune cells. Until now, it was not known how Tet proteins play a role in the development of autoimmune disorders.
Epigenetics deals with how reversible changes in DNA affect gene activity and protein expression. Disrupting this machinery can have dramatic effects on cellular function. The goal of our study was to understand how epigenetic control in a specific type of immune cells, called B cells, affects the development of autoimmune diseases.”
Tomohiro Kurosaki, Study Corresponding Author, Osaka University
To realize their objective, the team created a new mouse line in which the epigenetic regulator proteins—Tet2 and Tet3—are not produced by B cells. They observed a mild form of systemic lupus erythematosus, an autoimmune disorder, in the mouse line.
This disorder can affect the kidneys, skin, joints, and other organs, and there is no curative treatment available at present. Much like human patients, the mice presented with increased serum levels of autoantibodies as well as damage to their liver, lungs, and kidneys.
These findings suggest that Tet2 and Tet3, as well as proteins whose expression is regulated by Tet2 and Tet3, might play a fundamental role in the development of systemic lupus erythematosus. We wanted to gain a deeper molecular understanding of the mechanism behind the effects of Tet2 and Tet3 on the immune system.”
Shinya Tanaka, Study Lead Author, Osaka University
Then, the scientists examined another type of immune cell, known as T cells, which usually interact with B cells, and identified that T cells were highly activated in the Tet2/Tet3 knockout mice.
When the team analyzed the molecular interaction between the T cells and the B cells more closely, they observed that higher levels of CD86 protein were generated in B cells of the Tet2/Tet3 knockout mice, resulting in aberrant activation and autoimmunity of T cells.
These are striking results that show how Tet proteins suppress autoimmune diseases by inactivating B cells and thus ultimately preventing them from attacking our bodies.”
Tomohiro Kurosaki, Study Corresponding Author, Osaka University
“Our findings provide new insights into the contribution of epigenetics to the development of autoimmune disease. Regulating Tet proteins and their downstream effectors could be a novel treatment for autoimmune diseases,” Kurosaki concluded.
Source:
Journal reference:
Tanaka, S., et al. (2020) Tet2 and Tet3 in B cells are required to repress CD86 and prevent autoimmunity. Nature Immunology. doi.org/10.1038/s41590-020-0700-y.